The paradoxical surge of colorectal cancer (CRC) cases among younger adults is one of the biggest questions for oncology today. Now there is new evidence that an unexpected driver behind the mysterious rise of colon cancer cases in young adults is high blood-sugar levels.
This study found that young adults whose glucose levels were high were up to 65 percent more likely to be diagnosed with the cancer before age 50 than their peers. Diabetics were at the highest risk, but those with prediabetes—where blood sugar levels are higher than normal but not high enough to be classified as diabetes—were also at an elevated risk.
The new study was published in the Journal of the National Cancer Center. It was conducted by a group of researchers from Beijing, the Chinese Academy of Medical Sciences and Peking Union Medical College. The lead author is Chenyu Luo.
This study analyzed 374,568 participants from the UK Biobank cohort and 172,809 participants from the Kailuan cohort.
Researchers found, overall, a higher blood glucose level was associated with an increased risk of developing early colorectal cancer. Notably, elevated blood glucose levels were associated with an increased risk of CRC in a linear, dose-response manner. Also, elevated glucose (>7.0 mmol/L) was more strongly associated with young adult CRC than with older adult CRC.
Levels higher than 126 mg/dL were associated with a 61 percent increased risk of early-onset CRC compared to people with levels below 126 mg/dL among the U.K. cohort. Among the Chinese cohort, glucose levels higher than 126 mg/dL were associated with a 65 percent increased risk of early-onset colorectal cancers.
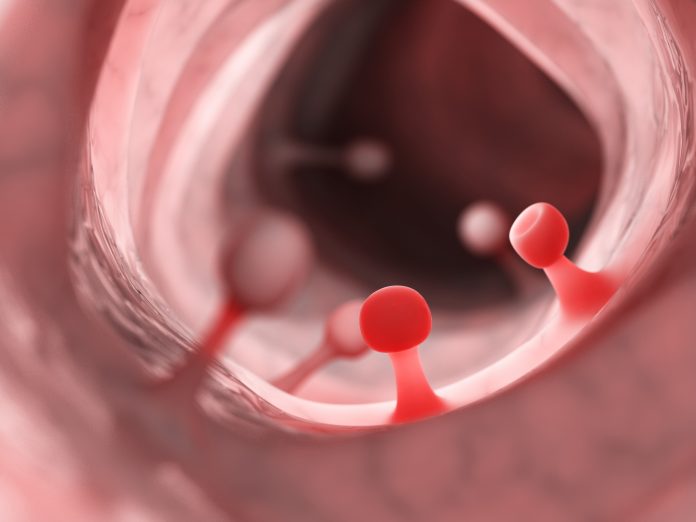
CRC is one of the most prevalent malignancies worldwide, accounting for approximately 10% of all cancer cases and is the second leading cause of cancer-related deaths worldwide. There were more than 1.9 million new CRC cases and 935,000 deaths in 2020. But it occurs mostly among older people. And its incidence in those above 50 years old has been decreasing globally in the last decades, probably as a result of better screening.
Meanwhile, from 1939, when the first case-reports of CRC in the young were published, the incidence of young adult CRC has been increasing and is expected to double by 2030. Young adult CRC exhibits differential epidemiological, clinical, pathological, and molecular features compared to late onset disease. But efforts to characterize young adult CRC, and to find out if it is a different entity from CRC in the older, have so far yielded no solid answers.
The authors write, “The mechanisms underlying the relationship between hyperglycemia and increased CRC risk involve direct effects of high glucose, metabolic advantages for cancer cells, insulin/IGF signaling dysregulation, and associated factors like oxidative stress, inflammation, and adipokine imbalance.”
First, high glucose concentrations can directly induce DNA damage independent of insulin in human endothelial cells, promote cell proliferation, enhance cancer-related signaling pathways like the Wnt/β-catenin pathway, and facilitate migration and invasion of CRC cells. Second, sustained hyperglycemia provides a metabolic advantage for cancer cells, which preferentially utilize glucose and divert glycolytic intermediates into biosynthetic pathways (the Warburg effect).”





