Diana Wei, a 59-year-old woman who never smoked a day in her life, was diagnosed with lung cancer after losing five pounds unexpectedly, and then another 13 pounds six months later.
Wei first dismissed her drop in weight to stress from moving from New York to California with her husband before the COVID-19 pandemic and starting a new job. But when she lost more pounds without changing her diet or exercise routine, she began to worry.
After informing her new doctor, Shih-Fan Sun, MD, at UCLA Health, about her weight loss, routine tests were done, however, everything came back normal.
Six months later, when Wei returned for a follow-up, she was 13 pounds lighter – prompting Dr. Sun to order a full-body scan.
Recounting what the doctor said a week later, Wei told UCLA Health, “He said, ‘I wanted to catch you before you leave for work. We saw something on the scan. I think you should reach out to a pulmonologist.’ That’s when I started to panic.”
Wei was in disbelief when she the scan found a lung nodule which led to her lung cancer diagnosis because she never smoked and always took preventative care measures for her body.
“When they told me I had lung cancer, my initial reaction was, ‘What are you talking about?’ I didn’t understand. At first, I was really quite angry. I did everything I was supposed to do. I always get my checkups,” she explained.
RELATED: You Never Smoked But Still Got Lung Cancer! Treatment Options May Be Different for You
She had regular mammograms and pap smears done “like clockwork,” she said, noting that her cholesterol and blood pressure were always within a healthy range.
According to thoracic surgeon Jane Yanagawa, MD, the number of non-smokers getting lung cancer has increased over the past few decades.
Yanagawa, of Jonsson Comprehensive Cancer Center, said Wei’s case “points out how much more research we need in figuring out risk factors and demographic factors to help provide the same screening benefit we are making with patients who have a smoking history, to see how we can expand that for patients who are never-smokers.”
She noted that occupational and environmental exposures, genetic susceptibility and exposure to second-hand smoke are also risk factors for lung cancer.
In Wei’s case, the cancer was caught early enough that a surgical treatment called a “segmentectomy” was successfully performed to remove cancerous tissue.
Dr. Yanagawa explained, “It was a minimally invasive lung cancer that was caught really early, for which she had a lung-preserving resection, due to the small size of it. Her life is not expected to be impacted by this. She is essentially considered to be cured.”
Wei, who is now clear of cancer nearly a year after her diagnosis, will have to follow up with regular CT scans to make sure another cancer doesn’t develop, Dr. Yanagawa said.
Now she has “a brand new outlook on life” and doesn’t take her “health for granted.”
“If it wasn’t for the weight loss, I would have continued doing what I was doing without a clue,” Wei said. “As women, we are so busy caring for our family and our work that we can kind of let things slide. But we have to be aware of our bodies and be vigilant – trust your instincts, and if something doesn’t feel right, tell your doctors and have it checked out.”
Understanding Lung Cancer
Lung cancer, the second most common type of cancer, is the leading cause of cancer deaths for men and women in the United States. Diagnosis and treatment of the disease can be tricky since symptoms often don’t appear until the cancer has spread.
An initial symptom, for example, could be as serious as a seizure if the lung cancer has already spread to the brain. But other symptoms can include increased coughing, chest pain, unexplained weight loss, shortness of breath, wheezing, losing your voice or persistent infections like bronchitis or pneumonia.
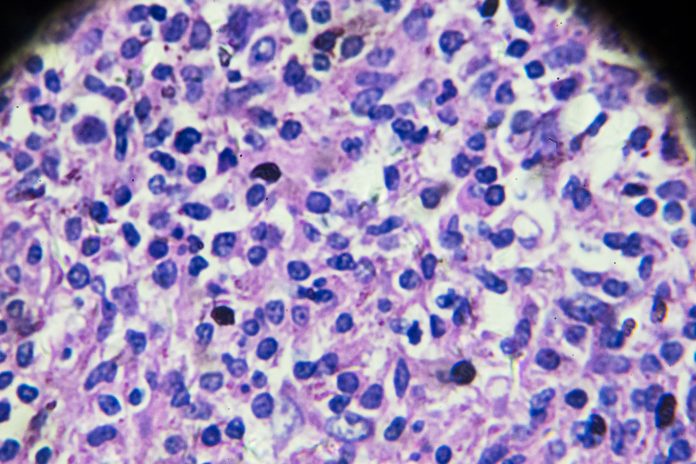
The two main types of lung cancer are non-small cell, which makes up 85 percent of cases, and small-cell. These types act differently and, accordingly, require different types of treatment.
Dr. Patrick Forde, a thoracic oncologist at Johns Hopkins Medicine, tells SurvivorNet about how distinguishing between the two types – and their subtypes – can be very beneficial.
What Happens When You’ve Been Newly Diagnosed With Lung Cancer
“Within that non-small cell category, there’s a subtype called non-squamous adenocarcinoma, and that’s the group of patients for whom genetic testing is very important on the tumor,” he explains. “Genetic testing is looking for mutations in the DNA, in the tumor, which are not present in your normal DNA.”
Surgery Options for Lung Cancer
There are several types of surgery for lung cancer, and the decision about which is best is based largely on the location of your cancer, its size and whether it has started to spread. A wedge resection is an option if the tumor is small and located on the outside of the lung. In this procedure, your surgeon removes a piece of the lung (in the shape of a wedge) and lung function is not affected.
By contrast, a lobectomy or a segmentectomy involves the removal of a certain segment of the lung (a lobe). During a pneumonectomy, however, the entire lung is removed.
Figuring Out Surgical Options for Lung Cancer Patients
There are several different ways to do lung cancer surgery. The standard operation used to be open surgery with a big incision in the chest and then spreading apart the ribs. But because of the pain after the operation and the lengthy recovery time, doctors are increasingly using less invasive operations including minimally invasive video-assisted thoracoscopic surgery (VATS) and robotic techniques.
Your surgeon will go over all of these options with you when planning your treatment.
Lung Cancer for Non-Smokers
Declining smoking rates have led to an improved outlook for lung cancer since cigarette smoking is the number one risk factor for the disease. In fact, the Centers for Disease Control & Prevention states that cigarette smoking is linked to about 80 to 90 percent of lung cancer deaths, and people who smoke cigarettes are 15 to 30 times more likely to get lung cancer or die from lung cancer than people who don’t smoke.
It’s important to remember, however, that even people who’ve never smoked before can still get lung cancer. The CDC reports that, in the United States, about 10 to 20 percent of lung cancers, or 20,000 to 40,000 lung cancers each year, happen in people who’ve never smoked.
“Some lung cancers are from unknown exposure to air pollution, radon, or asbestos,” Dr. Raja Flores, system chair of thoracic surgery at Mount Sinai previously told SurvivorNet in a previous interview. “We also see more never-smokers with lung cancer who have a family history of it.”
Radon is the second-leading cause of lung cancer. It’s responsible for anywhere from 3 to 16 percent of cancer cases depending on the levels present in a given area, according to the World Health Organization, but smokers are still 25 times more at risk from radon than non-smokers.
Another possibility for the cause of lung cancer in a non-smoker can be second-hand smoke. The American Cancer Society estimates that about 7,000 adults die of lung cancer annually from breathing secondhand smoke.
Air pollution, family history, HIV or AIDs can also all impact the chances of a non-smoker getting lung cancer. No matter what, it’s important to not rule out the disease just because you don’t smoke – a fact that Donna Hunting knows all too well.
Hunting was a non-smoker when she was diagnosed with lung cancer. But the active 54-year-old’s cancer had progressed further given that she had stage four non-small cell lung cancer.
If You Have Lungs, You Can Get Lung Cancer — Survivor Donna Hunting Shares Her Story
“That day was shattering to my family and to me,” she previously told SurvivorNet. “It’s not a smokers’ disease. If you have lungs, you can get lung cancer.”
Fortunately for Hunting, testing revealed that her tumors had a mutation in a specific gene called EGFR. This meant that doctors were able to give her a pill to block those mutations and effectively rid her body of the disease.
“After 50 days, miraculously, my PET scan showed no evidence of disease,” she said.
Hunting took the drug for over a year, until it stopped working as well. Now she’s on a different daily medication, but – thanks to advancements in treatment – she’s able to live with the disease.
“Cancer is a part of my life now, but it isn’t my whole life. I’m not letting cancer define me,” Hunting said.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet’s rigorous medical review process.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




