A study led by the Third Military Medical University in Chongqing, China, has identified three distinct molecular subgroups of non-alcoholic fatty liver disease (NAFLD) that are linked to disease severity and progression.
As reported in the journal Science Translational Medicine, patients classified as being in the first group (NAFLD-mSI) had mild symptoms; patients in the second group (NAFLD-mSII) showed macrophage infiltration into the liver and were at higher risk for cirrhosis of the liver; and those in the third group (NAFLD-mSIII) had increased risk of hepatocellular carcinoma and showed higher levels of gene expression of cancer-related genes.
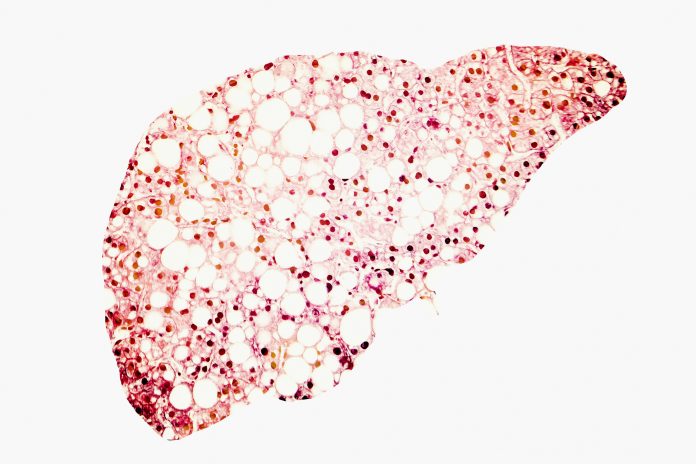
NAFLD is a common condition that affects around 25% of adults in the U.S. It occurs when excess fat builds up in the liver, making it harder for it to function as normal. NAFLD can progress to a more serious condition called metabolic dysfunction associated steatohepatitis or MASH (previously known as non-alcoholic steatohepatitis, NASH) in around 20% of people with NAFLD.
“The incidence of NAFLD is rapidly increasing and is becoming a common health care burden worldwide,” wrote first author Jingjing Ding, a researcher at the Third Military Medical University, and colleagues.
NAFLD and MASH are characterized by hepatic lipid accumulation and are associated with increased risk of cirrhosis or hepatocellular carcinoma. Although a treatment for MASH, resmetirom (Rezdiffra) developed by Madrigal Pharmaceuticals, was approved earlier this year it only works for around 30% of patients and the reasons for this are currently unclear.
“This lack of consistency is likely attributed to the high heterogeneity of human NAFLD, because the susceptibility to developing NAFLD is highly variable and influenced by a variety of risk factors, including aging, genotype, sex, ethnicity, dietary intake, bile acid metabolism, and insulin resistance,” wrote the authors.
To try and better characterize people with NAFLD, Ding and colleagues first tested a group of 103 people with this condition to look for molecular characteristics that could be indicative of different subtypes. They then validated their findings in a further group of 92 individuals with the same condition.
Using whole-genome sequencing, proteomics, phosphoproteomics, lipidomics, and metabolomics, the researchers discovered the three distinct groups of patients with NAFLD.
People in the NAFLD-mSI group had greater expression of CYP1A2 and CYP3A4, which act to prevent steatosis by regulating free fatty acid/bile acid–mTOR–FXR/PPARα signaling. People in the NAFLD-mSII group had higher risk of liver cirrhosis and liver infiltration of M1 and M2 macrophages linked to production of CCL2 and CRP in the liver due to fat buildup.
Finally, those in the NAFLD-mSIII group had greater expression of the cancer genes CEBPB and ERCC3 and were at higher risk for liver cancer as a result.
If further validated, the researchers hope their findings could help improve NAFLD diagnostics and allow better and more accurate predictions of how NAFLD will progress.
“By targeting these molecular subtypes of NAFLD through precision medicine strategies, it may be possible to reduce imprecision in NAFLD diagnosis and pharmacotherapy, potentially preventing its progression into cirrhosis and hepatocellular carcinoma in the early stages,” concluded the authors.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




