Beneath and beyond the reddish, flaky lesions that form in the skin of those with psoriasis, mild and severe forms of the disease can be told apart by the activity of key cells and signaling pathways, a new study shows.
Led by researchers at NYU Grossman School of Medicine, the study mapped hidden features of inflammation and how they compared in cases of increasing severity of psoriatic disease. The team’s findings may help explain how small areas of skin inflammation can have wide-ranging effects in other parts of the body. Up to one-fifth of those with the skin disease, the researchers note, go on to develop inflammation in the joints, or psoriatic arthritis. The study results, they say, may also offer clues as to why psoriasis can trigger this and other conditions, such as type 2 diabetes, heart disease, and inflammatory bowel disease.
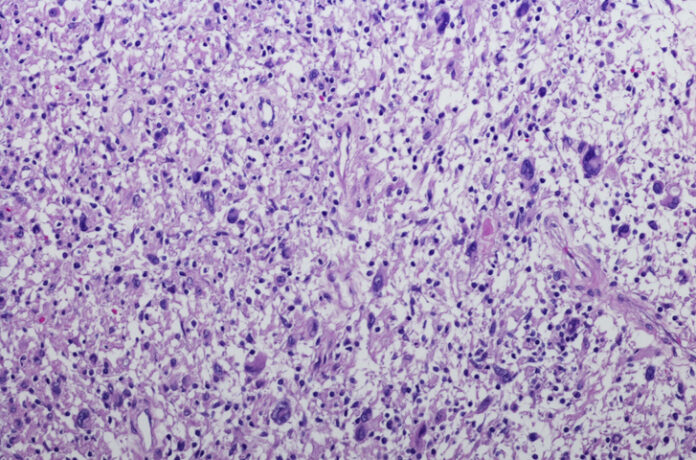
Published online June 2 in the journal Science Immunology, the new analyses revealed that the location of clusters of cells called fibroblasts, key regulators of inflammation, along with macrophages, a type of white blood cell, varied and were more common in upper layers of the skin in more-severe cases of psoriasis.
Further, the research team found that in skin samples from patients with moderate-to-severe psoriatic disease, gene activity increased in more than three dozen molecular pathways tied to metabolism and control of lipid levels, factors known to go awry in diabetes and cardiovascular diseases. This increased gene activity even occurred in clear skin far away from any lesions.
Our initial goal was to find measurable molecular signals that could tell us who is more likely to develop severe psoriasis, as well as who is at higher risk of developing related disorders that often accompany psoriasis, such as arthritis and cardiovascular disease.”
Jose U. Scher, MD, study co-senior investigator
“Having found signals with potential systemic consequences, we are now working to understand how skin inflammation can lead to widespread disease affecting other organs,” said Dr. Scher, the Steere Abramson Associate Professor of Medicine in the Department of Medicine at NYU Langone, where he also serves as director of the Psoriatic Arthritis Center and the Judith and Stewart Colton Center for Autoimmunity.
“Our study serves as a valuable resource for the scientific community, offering the most comprehensive archive of cellular and molecular features involved in both diseased and healthy skin,” added study co-senior investigator Shruti Naik, PhD. Dr. Naik is an assistant professor in the Departments of Pathology and Medicine and the Ronald O. Perelman Department of Dermatology at NYU Langone.
More than 8 million Americans, and 125 million people worldwide, are estimated to have psoriatic disease. The condition affects men and women equally.
Dr. Scher notes that the new study was designed to go beyond current diagnostic tools, which focus heavily on visible signs of skin lesions instead of looking at their invisible systemic and molecular effects. While many available therapies, including steroids and immunosuppressive drugs, reduce inflammation and symptoms, they do not address the underlying causes of the disease.
The new study relied on spatial transcriptomics, a technique that carefully charts the molecular and cellular interactions occurring in a specific tissue. Researchers analyzed intact skin samples from 11 men and women with mild to severe cases of psoriatic disease, plus 3 healthy adults without psoriasis. Spatial transcriptomics, they say, is more powerful than other commonly used techniques that track single cells because it creates a broad image-based map of where cells are located in tissues and the other cells with which they are communicating.
Dr. Naik says the team next plans to use their latest analysis to identify the biological mechanisms involved in skin inflammation in one area and how it affects skin or other organs in another part of the body. Further research is also planned in larger groups of patients and in lesioned and nonlesioned skin from the same patients to determine how disease clears on its own in some and why patients respond differently to the same anti-inflammatory medications.
For the benefit of researchers worldwide, study co-lead investigator and bioinformatician Ikjot Sidhu, MS, has archived the team’s spatial transcriptomics analysis on the website Zenodo: see “Spatial-HP-Skin” and “Spatial transcriptomics stratifies health and psoriatic disease severity by emergent cellular ecosystems.”
Funding support for the study was provided by National Institutes of Health grants P30CA016087, T32AR069515, UL1TR001445, DP2AR079173, R01AI168462, and UC2AR081029. Additional funding was provided by the National Psoriasis Foundation, the Judith and Stewart Colton Center for Autoimmunity, the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, the Beatrice Snyder Foundation, the Riley Family Foundation, and the Rheumatology Research Foundation, as well as the New York Stem Cell Foundation.
Dr. Naik serves on the advisory boards of Seed Inc. and as a consultant for BiomX. She also receives research funding from Takeda Pharmaceuticals. Dr. Scher has served as a consultant for Janssen, AbbVie, Novartis, Pfizer, Sanofi, UCB, and BMS. He also receives research funding from Janssen and Pfizer. Study co-investigator Andrea L. Neimann, MD, serves as a consultant for Janssen, UCB, AbbVie, and BMS. Study co-investigator John A. Carucci, MD, PhD, also receives research funding from Regeneron, Sanofi, and Genentech.
All of these arrangements are being managed in accordance with the policies and practices of NYU Langone.
Source:
Journal reference:
Castillo, R. L., et al. (2023) Spatial transcriptomics stratifies psoriatic disease severity by emergent cellular ecosystems. Science Immunology. doi.org/10.1126/sciimmunol.abq7991.