A new study conducted by researchers at the Albert Einstein College of Medicine indicates that the COVID-19 pandemic has led to a significant increase in the risk of dyslipidemia, a condition characterized by abnormal lipid levels in the blood. The research, which analyzed data from more than 200,000 adults, found that the risk of developing dyslipidemia rose by 29% during the pandemic. The research, published in The Journal of Clinical Investigation, also showed that older adults and individuals with type 2 diabetes experienced nearly double the risk of dyslipidemia compared with the general population.
“Given the extent of the pandemic, this increase in dyslipidemia risk is a cause for concern around the world,” said study leader Gaetano Santulli, MD, PhD, an associate professor of medicine and molecular pharmacology at Albert Einstein. “Based on our findings, we would advise people to have their lipid levels monitored regularly and to consult with their healthcare providers about ways to treat dyslipidemia if detected, especially elderly individuals and patients with diabetes.”
Santulli noted that this advice should apply to all adults not just those who received a positive COVID-19 diagnosis, as it is known that a significant portion of the population were infected but didn’t realize it as they never exhibited symptoms.
Prior to the pandemic, it was estimated that just over half the population of adults in the U.S., or about 53% of had dyslipidemia. With a 29% surge in risk tied to the COVID-19 pandemic, this could mean that more than two-thirds of the population—about 68%—are at risk of developing lipid abnormalities in the blood.
In two previous studies, Santulli and colleagues had identified increased rates of hypertension and type 2 diabetes associated with COVID-19. They showed an elevated risk of developing these health conditions as long as three years after the pandemic. They also observed a “suspicious” increase in total cholesterol levels among people, which spurred this new research.
The current study assessed the incidence of dyslipidemia in a cohort of 200,000 people from Naples, Italy, comparing data from three years before the pandemic (2017–2019) with data from the pandemic period (2020–2022). The analysis excluded individuals who had been previously diagnosed with dyslipidemia or were on lipid-lowering medications.
The results showed a 29% increase in dyslipidemia risk across the entire study group, with higher increases in people 65 and older, as well as those with pre-existing health conditions such as diabetes and obesity.
“Our study did not attempt to determine whether participants had tested positive for COVID-19,” Santulli noted. “Instead, we were able to measure COVID’s overall impact on the population by simply comparing levels of dyslipidemia before and after the pandemic.”
The researchers believe that the rise in dyslipidemia may be linked to the broad disruptions caused by COVID-19, which potentially affected not only those who were infected, but the general population as well. The study leveraged a unique aspect of healthcare in Italy, where every citizen has a primary care physician which allowed for a more comprehensive, population-based analysis of health data.
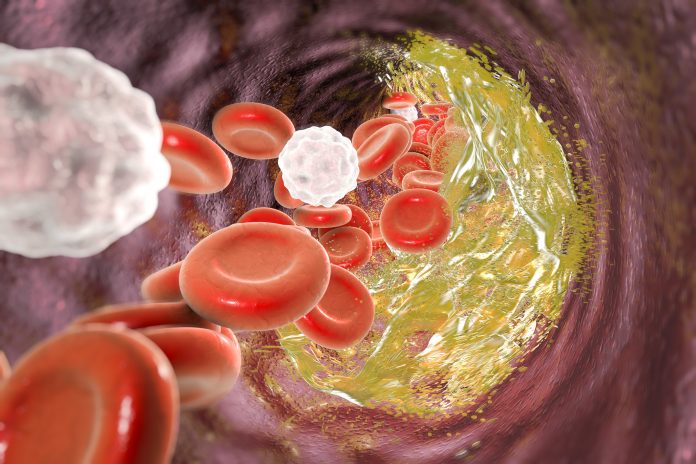
While the mechanisms by which the COVID-19 pandemic has influenced dyslipidemia risk are unclear, Santulli surmised that the virus may disrupt endothelial cells, which are critical for regulating blood lipids. Previous studies have also indicated that COVID-19 can elevate the risk of heart attacks and strokes, further implicating dyslipidemia as a contributor to cardiovascular disease.
The implications of these findings extend beyond individual health, raising concerns about the broader effects on healthcare systems. The pandemic’s impact on lifestyle changes—such as stress, altered diets, and reduced physical activity—might also play a role in increasing lipid levels. The team is now investigating the long-term effects of COVID-19 on cardiovascular-kidney-metabolic (CKM) syndrome, a recently described condition connected to four medical conditions of heart disease, kidney disease, diabetes, and obesity, all of which are influenced by endothelial dysfunction.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




