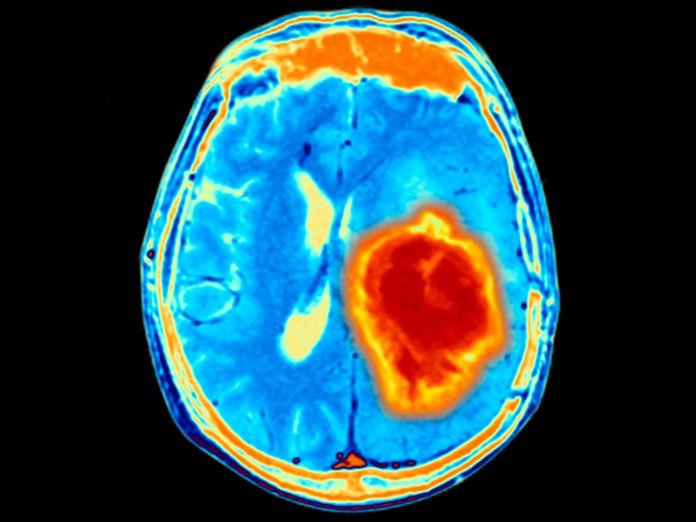
Brain metastasis remains one of the most challenging and deadly complications of cancer. In new research from McMaster University, a team has revealed a new way to prevent cancer cells from migrating to the brain.
Jakob Magolan, a medicinal chemist, PhD, collaborated with neurosurgeon Sheila Singh, PhD, on this work which focuses on brain metastasis-initiating cells (BMICs) and the development of selective inhibitors to target these cells before they lead to full-blown brain tumors.
The discovery of brain metastasis-initiating cells
The foundation of this project lies in Singh’s discovery of BMICs. These rare cells are responsible for seeding metastasis in the brain, particularly in cancers like lung, breast, and melanoma. By reinjecting human cancer cells into mice and observing their migration to the brain, Singh’s team previously identified these cells as key drivers of metastasis.
“The gene expression profile in those cells is very unique, and that was the sort of trigger point for looking for vulnerabilities and small molecules to target them,” Magolan explained.
With this knowledge in hand, the team began exploring ways to selectively target these BMICs, setting the stage for the development of new treatments that could potentially prevent brain metastasis before it becomes untreatable.
Targeting the enzyme IMPDH
The next step in the project was identifying a molecular target. Using gene expression profiles, the team turned to connectivity mapping that allows them to predict which small molecules could reverse the gene expression patterns found in BMICs. The focus fell on a specific enzyme: inosine monophosphate dehydrogenase (IMPDH). IMPDH plays a crucial role in the synthesis of nucleic acids, which are needed for cell division.
IMPDH has two isoforms, and while there are existing drugs, such as mycophenolic acid (MPA), that inhibit this enzyme, they are not suitable for this application due to issues with blood-brain barrier permeability and lack of selectivity between the isoforms.
Thus, Magolan’s lab initiated a medicinal chemistry program aimed at developing new compounds with greater selectivity and the ability to cross the blood-brain barrier.
“We needed to make a new one, a fundamentally novel scaffold,” he explains, which is the focus of this paper.
Developing new IMPDH inhibitors
The team has already made significant progress, synthesizing over 500 new compounds in their quest to find the right IMPDH inhibitor. Of these, several have shown promise in terms of potency and blood-brain barrier penetration.
Although the work is still ongoing, the potential impact of this discovery is significant. “The ability to inhibit BMICs early, before metastasis is detectable, could dramatically improve patient outcomes,” Magolan explains. “Once brain metastases form, they’re very treatment-resistant. Surgery is often not an option, and existing therapies can only prolong life by a few months.”
One of the most exciting aspects of this research is the potential for a preventative treatment. The team envisioned a drug that could be administered to patients after their primary cancer treatment, targeting any remaining BMICs that could cause future metastasis.
“We are hypothesizing a 12- to 16-month administration of this compound post-lung cancer, even if the lung cancer is cleared. That will prevent metastasis formation,” Magolan says.
The team believes this approach could be particularly effective for cancers that are prone to metastasizing to the brain, such as lung cancer, where 20% of patients experience brain metastasis within 12 months of being declared cancer-free.
The team is preparing to form a spin-off company at McMaster to license the intellectual property and translate this work by developing these compounds and moving toward clinical trials.
By targeting BMICs before they can seed brain tumors, the team believes this approach offers the possibility of preventing a currently untreatable complication of cancer.
“This is a really innovative strategy,” said Magolan. “The clinicians we’ve spoken to love it, and if we can get the molecule to work as promised, I think the path to the clinic is what’s really exciting.”





