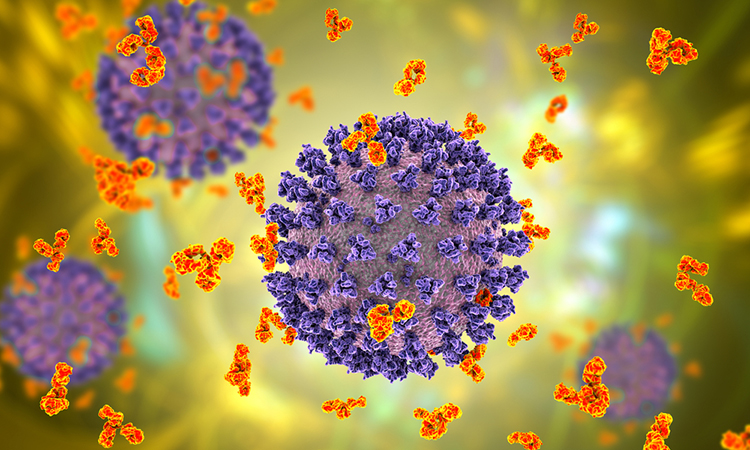
US researchers find that SARS-CoV-2 bivalent antibodies can continue to neutralise Omicron and Omicron lineages.
A new study led by scientists at La Jolla Institute for Immunology (LJI), US, showed how ideal antibodies against SARS-CoV-2 hit their marks.
Instead of targeting a single binding site on the SARS-CoV-2 Spike protein, these powerful antibodies bind to two of these sites at once. Through this “bivalent” binding, the antibodies can lock key viral structures into position, preventing the virus from infecting host cells.
The new findings, published in Cell Reports, suggest bivalent antibodies retain efficacy against both early SARS-CoV-2 variants and several later Omicron variants. Now, the scientists are looking at how we might harness their power in new antibody therapeutics and even more effective COVID-19 vaccines.
Current COVID-19 vaccines are designed to teach the body to recognise the SARS-CoV-2 Spike protein. Spike is important because it recognises and latches onto host cells through a region called the receptor binding domain (RBD). Each spike has three copies of the RBD. An antibody that can bind to a target (called an epitope) on the RBD has a chance to jam up this machinery and stop infection.
The problem is that SARS-CoV-2 keeps mutating, and many once-powerful antibodies cannot recognise their usual targets on RBDs. Building vaccines and therapies that will withstand future variation both hinge on figuring out what surviving antibodies have in common.
The researchers analysed nearly 400 antibodies sent by scientists around the world to the CoVIC, which is headquartered at LJI. They narrowed down this huge pool and found 66 potent antibodies that could neutralise Omicron lineage BA.1 and early sub-lineages such as BA.1.1 and BA.2. By the time they tested antibodies against Omicron lineages BA.4/5, only seven antibodies had neutralising power.
The broad scope of the CoVIC antibody panel comprising hundreds of therapeutic candidates contributed by over 60 groups in both corporate and academic settings—combined with side-by-side comparisons using a range of techniques—revealed enough of this rare antibody population to explain what features made them special.
“It became clear there was a pattern,” said Dr Heather Callaway. “The successful antibodies overcome loss of affinity for Omicron by simultaneously binding two RBDs in the Spike.”
The best neutralising antibodies did not bind their targets, one at a time, especially strongly, but by locked together two adjacent RBDs at once, even Omicron had a tough time escaping. Bivalent binding equalled antibody survival against the latest variants.
The LJI team has shown the importance of imaging the intact, complete antibody as it exists in nature, a type of analysis only possible with new and powerful electron microscopes. By doing so, the team could distinguish what survived compared to what fell to the wayside upon emergence of Omicron. Antibodies that use both their arms to anchor two RBDs at once withstood viral evolution.
Going forward, the researchers will continue to test the CoVIC pool of antibodies against new SARS-CoV-2 variants. This information is essential to development of better vaccines – that will elicit immunity that lasts multiple seasons of viral evolution.
Learning more about these antibodies can guide creation of next-generation antibody cocktails that are more resistant to ever-emerging SARS-CoV-2 variants.
The LJI researchers also say it is critical to look at how new vaccines present the Spike protein to the immune system. The more accurate the immunogen version of Spike is, and the more accurately it presents the arrangement and spacing of the component parts, the more likely it will elicit neutralising antibodies.










![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




