
Researchers at McMaster University have discovered a novel population of immune cells that may play a significant role in the worsening of asthma symptoms, particularly in patients with severe forms of the condition. The study, published in Science Translational Medicine, found that immune cells called “intermediate ILC2s” are linked to the presence of two types of cells—eosinophils and neutrophils—known to exacerbate asthma symptoms.
“When you can’t breathe, nothing else matters,” said senior author Roma Sehmi, PhD, a professor in the division of respirology, department of medicine at McMaster University. “We sought to better understand the mechanisms behind severe asthma so that we can better treat these patients.”
Severe asthma affects up to 10% of asthma sufferers and is notoriously difficult to treat because it does not respond well to standard therapies such as glucocorticosteroids. This new discovery provides a new target for treatment that could benefit the cohort of people with asthma who experience severe symptoms.
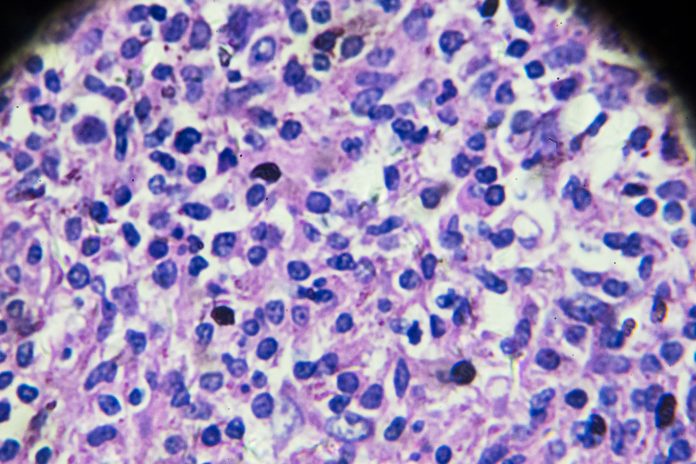
The research team, including members from McMaster University and St. Joseph’s Healthcare Hamilton, focused on a previously unidentified group of immune cells in the airways of patients with severe asthma. These cells called c-kit+IL-17A+ ILC2s are likened by the research team to chameleon because they can change their characteristics, adopting features of another type of immune cell. The presence of these cells, which are associated with neutrophil accumulation in the airways, was found to correlate with the severity of asthma symptoms. Further, these cells are much less responsive to standard asthma treatments.
By examining these cells in greater detail, the researchers discovered that “intermediate ILC2s” were most abundant in patients with severe asthma exhibiting mixed granulocytic inflammation, which includes both eosinophils and neutrophils. These cells are associated with high levels of IL-1β and IL-18, inflammatory proteins that promote the activation and accumulation of neutrophils in the airways. This finding suggests that controlling the number of intermediate ILC2s could help reduce neutrophil buildup and alleviate severe asthma symptoms.
“When asthma is associated with both eosinophils and neutrophils cells, individuals are generally less responsive to treatment with glucocorticosteroids,” said Parameswaran Nair, PhD, co-corresponding author and professor in the department of medicine at McMaster University. “The findings from this research pave the way for discovering new therapeutic targets for difficult-to-treat asthma.”
The researchers also identified specific growth factors that promote the formation of these intermediate ILC2s. By controlling the number of these cells, it may be possible to prevent neutrophil accumulation and reduce the severity of asthma symptoms in patients who are resistant to current therapies.
The study is built on more than a decade of collaborative research by Sehmi’s and Nair’s labs, with significant contributions from Xiaotian (Tim) Ju, PhD, the study’s first author, who recently completed his PhD in Sehmi’s lab and is now a postdoctoral fellow at the National Institutes of Health.
The study adds to the growing evidence that a more nuanced understanding of immune cell behavior is crucial in developing treatments for complex respiratory diseases like asthma.








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




