A novel technique developed by researchers at the Washington University (WashU) School of Medicine has allowed them to study aged neurons in the lab without the need for a brain biopsy. The technique has identified aspects of the genome of cells in the development of late-onset Alzheimer’s disease (AD) that may pave the path for new targeted treatments.
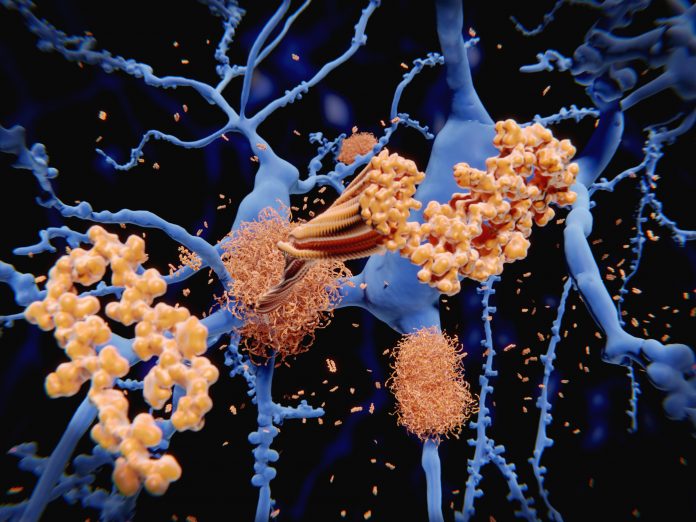
According to research published today in Science, the team took skin cells from patients with late-onset AD and transformed them into neurons. The investigators showed, for the first time, that lab-derived neurons accurately reproduced the known indications of AD, such as buildup of amyloid beta, tau protein deposits, and cell death.
With a working model of the disease, the researchers say they have found that aspects of the cells’ genomes called retrotransposable elements, which are known to change their activity as people age, are implicated in the development of late-onset AD.
“Sporadic, late-onset Alzheimer’s disease is the most common type of Alzheimer’s disease, representing more than 95% of cases,” said senior author Andrew Yoo, PhD, a professor of developmental biology at WashU. “It has been very difficult to study in the lab due to the complexity of the disease stemming from various risk factors, including aging as an important contributor. Until now, we did not have a way to capture the effects of aging in the cells to study late-onset Alzheimer’s.”
Until now, the study of the disease has focused on mouse models with rare genetic mutations that are known to be the cause of inherited, early-onset AD, which occurs in younger people. These mouse studies have provided useful data on AD, but it differs from the disease development pathway for the 95% of people with the late-onset form.
To overcome this, the team in the Yoo lab used a novel, direct cell reprogramming technique that bypasses the stem cell stage allowing the skin cells to be directly transformed into neurons. This allows the cells to retain the characteristics of cellular aging. Yoo’s team had previously used this same technique using microRNAs in a study of Huntington’s disease.
Once the transformation of the cells was completed, the researchers noted that they would group into small clusters, or spheroids, that mimic the three-dimensional aspects of the brain. For their study the team compared the spheroids of late-onset AD, inherited AD, and those of healthy people.
The spheroids of AD patients soon showed the formation of amyloid beta deposits and the characteristic tau tangles between neurons that are hallmarks of the disease. Activation of genes associated with inflammation also occurred followed by neuronal death, the same that has been observed via brain scans of AD patients. Spheroids of the older, healthy patients also showed some amyloid beta deposits, but at a much lower level suggesting that these deposits and tau accumulation are merely factors of aging.
The investigators also looked to treat the neuronal cells from the late-onset patients with drugs that are known to interfere with amyloid beat plaque formation. When they treated the cells early in the development of disease, amyloid beta buildup was lessened significantly, but later treatment—once some amyloid beta buildup was present—had more muted response and only modestly prevented additional amyloid beta deposits. This finding highlights the importance of early identification and treatment of AD.
Further research showed that retrotransposable elements—so called “jumping genes”—play a role in late-onset AD development. Inhibiting these elements with the anti-retroviral drug lamivudine, which is know to hinder the activity of retrotransposable elements showed good results. The neuronal spheroids from late-onset patients exhibited lower amyloid beta levels, reduced tau tangles and lower levels of neuron death compared with the same spheroids treated with placebo. Further, treating the spheroids from early-onset AD patients with lamivudine showed no benefit, showing that the two forms of the disease have distinct molecular features.
“In these patients, our new model system has identified a role for retrotransposable elements associated with the disease process,” Yoo said. “We look forward to using this model system as we work toward new personalized therapeutic interventions for late-onset Alzheimer’s disease.”





