A new way of selecting treatments for terminal pancreatic cancer patients may have been uncovered by researchers at the University of Birmingham and collaborators.
Using cells from twelve patients, the research team created a single-cell map of tumor-infiltrating immune cells and peripheral immune cells, coupled with gene expression, single-cell TCR and BCR sequencing, and identifying proteins expressed on these cells. The team then verified their findings using two other large publicly available pancreatic cancer datasets.
Their work was published in Nature Communications. The lead author is Shivan Sivakumar, PhD, FRCP, of the University of Birmingham.
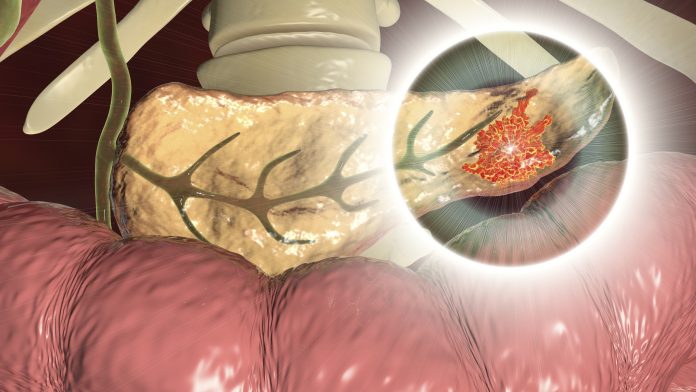
Pancreatic ductal adenocarcinoma (PDAC) has the worst survival of any common human cancer, with a five-year survival of below 10%. Approximately 15% of patients benefit from surgical resection, which can cure a subset of those patients. The benefit of immunotherapy in PDAC is minimal.
This study shows why there are differences in prognosis between different pancreatic tumors and identifies potential avenues for improved treatment approaches. Some tumors may potentially be more susceptible to macrophage-based therapies.
“We demonstrate the need for trials to assess changes in immune infiltration over time. Collectively our data provides a foundation for understanding the failure of immunotherapy in pancreatic cancer with an avenue for designing novel therapeutics and tailored interventions,” said Sivakumar.
Rachael Bashford-Rogers, PhD, associate professor of molecular and cellular biochemistry from the University of Oxford and a senior author of the study said: “We have uncovered distinct immune environments in pancreatic cancer, revealing new therapeutic opportunities to improve outcomes for this deadly disease. By leveraging single-cell multi-omics and novel computational approaches, this study identifies potential strategies such as boosting certain cell responses, and depleting suppressive immune cells to enhance immune-based treatments.”
The study also uncovered an important understanding of the role of specific immune cells, such as activated regulatory T cells (Tregs) and B cells, in the immunopathology of this disease. The team found that these cells could help to distinguish patients who may benefit from targeted treatments that activate the existing immune response in the tumor area (rich in B and T cells) versus those that have a highly suppressive tumor environment (rich in myeloid cells). Tackling these cells would play an important therapeutic strategy in the future against this disease.
As a result, potential targets have been identified with more weight being given to the target TIGIT which was previously identified as a target of interest in this disease and now this work also suggests that CD47 can be targeted too. The work also suggests strategies to boost B cell responses, target immunosuppressive macrophages, and deplete activated intratumoral Tregs which will be of benefit to different subsets of patients, and these are now fertile areas to investigate.
Pancreatic cancer is among the deadliest cancers globally, with a survival rate beyond 10 years of less than 1% in England (2013–2017). It is often only when the cancer has reached an advanced stage that physical symptoms appear, at which point it becomes more difficult to treat.
“Sadly, pancreatic cancer is typically diagnosed at a late stage, when curative surgery is no longer an option. The problem is exacerbated by the fact that for the ‘lucky’ 1 in 10 who are eligible for surgery, the recurrence rate of pancreatic cancer after surgical treatment is over 80%,” said Sivakumar.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




