A new study comprehensively maps tumor genes that are self editing to avoid immune attack, providing a roadmap for designing better immunotherapies. A team of researchers found that late tumors used gene editing to suppress antitumor immunity genes, reducing infiltrating immune cells and tumor–immune cell communications.
Further, the team found immune gene repression in tumors was reversed by inhibiting DNA methylation using low-dose decitabine, which suppressed tumor growth and restored immune control. It also increased the number, functionality and memory of tumor-infiltrating lymphocytes and reduced the number of myeloid suppressor cells.
The findings were published in Nature Immunology. The lead author is Judy Lieberman, MD, PhD, in the Program in Cellular and Molecular Medicine (PCMM) at the Boston Children’s Hospital.
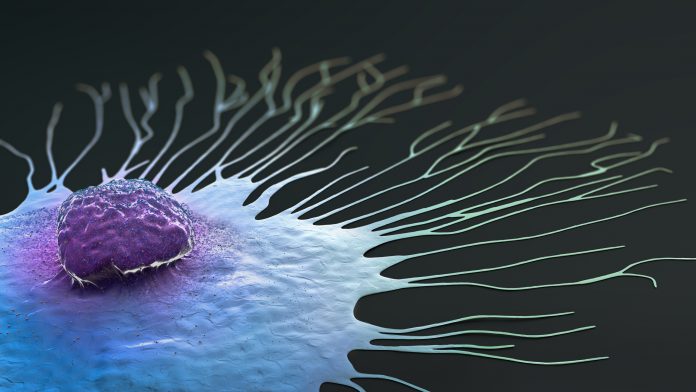
Cancer cells edit their gene expression to evade immunosurveillance. In this study, innate immune genes, especially interferon-stimulated genes, dominated the list of downregulated tumor genes, while genes that regulate cell-intrinsic malignancy were mostly unedited. Naive and activated CD8+ T cells in early tumors were replaced with exhausted or precursor-exhausted cells in late tumors.
Immunotherapies such as CAR-T cells and checkpoint inhibitors can strengthen the immune system’s attack against cancer. But they don’t work for most solid tumors.
This study used single-cell RNA sequencing in a breast cancer genetically engineered mouse model (GEMM) to identify edited genes.
To capture how cancers edit genes, the researchers tracked breast tumors from their origins. After turning on the Her2 oncogene in their mouse model, they used genome-wide single-cell RNA sequencing to identify which genes the newly-formed tumor was editing. They did this twice—one week and one month after Her2 oncogene induction.
Many of the genes the tumors edited are involved in the innate immune response— including those that are stimulated by interferon and that enable immune cells to recognize tumor signals. Tumors silenced these genes epigenetically, primarily by chemically modifying the genes’ promoter sequences through methylation.
Notably, the tumors edited relatively few genes associated with enhanced proliferation. “While the tumor also mutates to become more malignant, the dominant changes were immune,” said Lieberman, in a Children’s Hospital release.
To reverse tumor editing, Lieberman and her colleagues used an existing FDA-approved methylation inhibitor, decitabine. At low doses, decitabine reactivated the immune response, restoring multiple facets of immune control over the tumor and reducing tumor growth.
The researchers saw an increase in T cells, natural killer cells, and dendritic cells and a sharp reduction in immunosuppressive myeloid-derived cells. Studying implanted breast and melanoma tumors, they found that decitabine restored function of genes involved in the innate immune system’s danger signaling pathways. These included pathways involving interferons or an inflammatory cell-death pathway known as pyroptosis.
Their current study involved a breast cancer model, but Lieberman believes that gene editing is common to all cancers. Her lab plans to further validate its results and test decitabine, already used in some leukemias, in other solid tumors such as lung and ovarian cancer.
Lieberman also wants to study patients with genetic predispositions to cancer, who get screened frequently, to catch tumors in their earliest stages. “We hope to get tumor tissue from those patients and do what we did in the mice,” she said, in the Children’s Hospital release.





