A molecular imaging approach can distinguish between different types of a common ovarian cancer and rapidly predict its response to chemotherapy within just 48 hours.
The technique, based on magnetic resonance imaging (MRI), could allow physicians to personalize treatment within days as opposed to the usual weeks or months.
Hyperpolarised carbon-13 imaging swiftly revealed whether a tumor was receptive or resistant to standard, first-line Carboplatin chemotherapy in cell models of high-grade serous ovarian cancer.
The research revealing how this noninvasive imaging method might be used is published in the journal Oncogene.
“We can image a tumor pre-treatment to predict how likely it is to respond, and then we can image again immediately after treatment to confirm whether it has indeed responded,” said senior researcher Kevin Brindle, PhD, a professor at the University of Cambridge.
“This will help doctors to select the most appropriate treatment for each patient and adjust this as necessary.
“One of the questions cancer patients ask most often is whether their treatment is working. If oncologists can speed their patients onto the best treatment, then it’s clearly of benefit.”
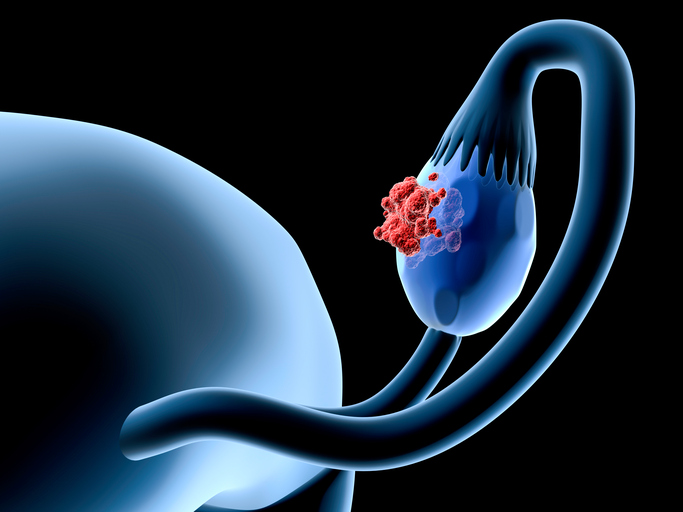
Ovarian cancer is a leading cause of cancer-related deaths in women, with the most common lethal form being high grade serous ovarian cancer.
It presents as two metabolic subtypes: a high OXPHOS subtype shows increased expression of genes encoding electron transport chain components, increased oxygen consumption, and increased chemosensitivity whereas a low OXPHOS subtype exhibits glycolytic metabolism and is more drug resistant.
In the current study, researchers examined whether clinically applicable metabolic imaging methods could be used to discriminate between different gene copy number signatures and between high and low OXPHOS metabolic subtypes.
Gene copy number signatures have previously been revealed to have prognostic significance in ovarian cancer and have the potential to be used in treatment selection as they discriminate between different mutational processes.
The researchers used patient-derived ovarian cancer organoids and xenografts of high-grade serous ovarian cancer to detect early response to treatment before there were any changes in tumor volume.
They found that patient-derived xenografts representative of different metabolic subtypes showed differences in glycolytic metabolism that could be detected using hyperpolarized carbon-13 imaging, which involves injecting a labelled form of the naturally occurring molecule pyruvate and showing its rate of metabolism into lactate.
By contrast, there were no significant differences in uptake of the radioactive tracer fluorodeoxyglucose determined using positron emission tomography (PET), which is widely used in clinical practice.
Amplification of the Myc gene was the likely mechanism driving increased lactate labeling relating to the low OXPHOS metabolic subtype. However, there did not appear to be a correlation between the metabolic and growth behavior and copy number signatures with the low OXPHOS subtype.
Both the PET and hyperpolarized scans could detect response in a high OXPHOS tumor that was sensitive to Carboplatin treatment and non-response in a low OXPHOS tumor that was drug resistant.
The researchers anticipate that hyperpolarized carbon-13 imaging will be trialled in ovarian within the next few years.
“This technique tells us how aggressive an ovarian cancer tumor is and could allow doctors to assess multiple tumors in a patient to give a more holistic assessment of disease prognosis so the most appropriate treatment can be selected,” Brindle said.





