Research led by teams in Lausanne, Switzerland has developed a chimeric antigen-receptor (CAR)-T cell therapy that can be switched on and off using readily available existing drugs.
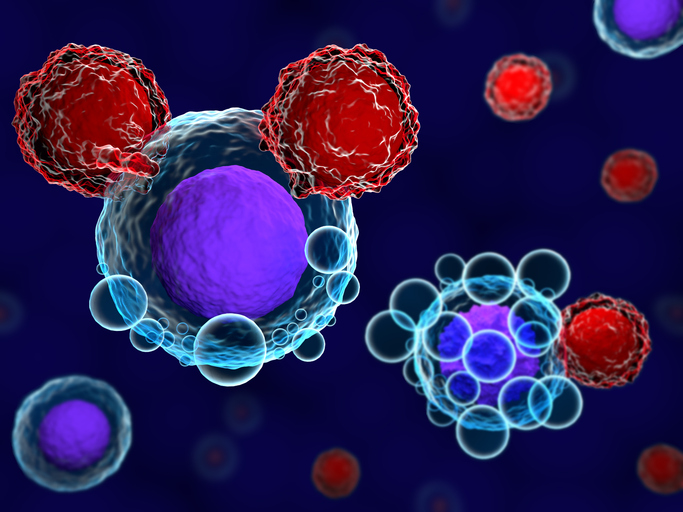
CAR-T cell therapies are a type of cancer immunotherapy where T cells are engineered to better target the cancer cells of interest. These mostly involve a patient’s own cells, which are extracted, engineered and reintroduced to the body to target the patient’s cancer.
CAR-T cell therapies have been used successfully to treat advanced “liquid” cancers such as leukemia and lymphoma. Several are approved, but treatment of “solid” tumors, such as breast, lung, or prostate cancer, among others, with these therapies has proved challenging.
“CAR-T cells are already used today to treat a number of blood cancers, but solid tumors continue to pose significant challenges for this mode of therapy in terms of both safety and efficacy,” said co-lead author Melita Irving, PhD, a researcher at the Ludwig Institute for Cancer Research, Lausanne, in a press statement.
“We have potentially addressed both these issues by engineering, directly into the CAR design, on and off switches that are engaged by drugs that have been approved by regulatory agencies and are already in use in the clinic. This should hasten the advancement of these remotely controlled CAR-T cells into clinical trials.”
The study, recently published in PNAS, is at an early stage, but showed the newly engineered CAR-T cell therapy could be switched on using venetoclax and switched off within a few hours by lenalidomide. Both these drugs are oral cancer drugs that are already approved.
The researchers essentially added an extra segment to the CAR receptor that needs venetoclax to activate the anti-cancer activity of the receptor and allow it to home in on cancer cells. Similarly, an additional segment added to the receptor allows the cell to be marked for disposal by the body’s waste disposal machinery when exposed to lenalidomide.
“Having the ability to remotely switch CAR-T cells on to varying degrees using different doses of an activating drug—and then off on demand, as needed—would improve the safety of this therapy,” said first author Greta Maria Paola Giordano Attianese, PhD, also based at the Ludwig Institute. “Further, the remote control of CAR-T cell activity could also be used to mitigate T cell exhaustion, improving the durability of patient responses to the therapy.”
So far, the potential therapy has only been tested in preclinical studies, so it may be some time before they reach the clinic, but the research team now plans to advance their potential therapy further and to assess if it will indeed improve the performance of currently available CAR-T cell therapies that do not allow remote control via on/off switches.





