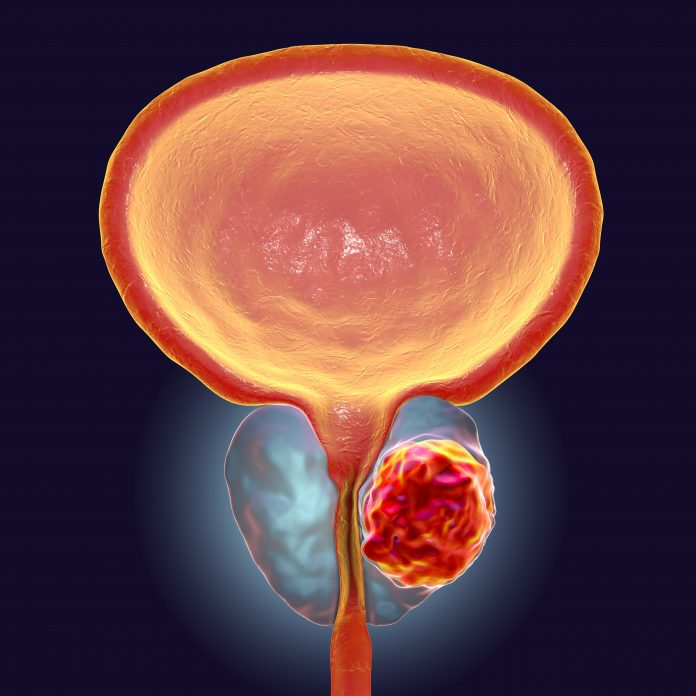
New research from the University of Michigan has shed light on a pivotal protein, NSD2, and its role in promoting prostate cancer.
NSD2 is a histone methyltransferase, a protein responsible for modifying histones—proteins around which DNA is wrapped. This modification influences the accessibility of DNA, ultimately affecting gene expression. In healthy prostate tissue, NSD2 is not expressed. However, in cancerous states, it is abnormally gained, where it appears to play a key role in driving the aggressive behavior of cancer cells. “NSD2 is a cancer-specific collaborator of the androgen receptor that essentially rewires its activity to support prostate cancer development,” said Abhijit Parolia, PhD, first author of a new paper in Nature Genetics.
The team’s findings reveal that NSD2 reprograms the function of the androgen receptor (AR), a protein that is crucial for normal prostate development and function. Under normal conditions, the AR halts cell proliferation and ensures that prostate cells perform their specific functions, such as secreting prostatic fluid. However, when NSD2 is expressed in cancer cells, it alters the AR’s activity, causing it to promote uncontrolled cell division. “This is the first molecular explanation for how that anti-proliferative, normal AR gets converted into a pro-proliferation, cancerous, oncogenic AR,” Parolia noted.
“Only when you get a malignant state do you see NSD2 expression,” says Parolia. “What’s even more interesting is we found an even higher induction and expression of this protein as the tumor becomes more aggressive and gains the ability to leave the primary site and go to seed a metastatic secondary lesion.”
To understand how NSD2 exerts its cancer-driving effects, the researchers conducted a CRISPR screen to identify proteins involved in the AR and prostate cancer pathway. They discovered that NSD2 reorganizes the “enhanceosome,” a complex of proteins a complex of multiple proteins, including transcription factors and other epigenetic factors, that assemble on the DNA at specific sites to drive the expression of genes that normally regulate healthy cells. By rearranging the location of the AR enhanceosome on DNA, NSD2 drives the AR to bind to cancer-causing genes and activate their expression.
NSD2 essentially rewires the DNA landscape, allowing the AR to activate new regions of DNA called enhancers. Enhancers are DNA elements that increase the expression of genes, and in cancer cells, NSD2 significantly increases the number of active enhancers. “If a cell has only 10 enhancers, this molecule, when expressed, makes it have 50 enhancers in total,” Parolia explained. This drastic increase in DNA activity enables cancer cells to hyper-divide, invade surrounding tissues, and metastasize to distant organs.
The research team also developed a first-generation drug that degrades both NSD2 and its closely related protein, NSD1, which is similarly implicated in cancer progression. The drug uses a proteolysis-targeting chimera (PROTAC) mechanism, a technology designed to tag specific proteins for degradation.
The bifunctional PROTAC drug binds to both NSD1 and NSD2 and then brings it to the proteasome to degrade it. So it functionally inactivates by degrading both NSD one and two in tandem. Parolia says, “The normal cells don’t respond, primarily because these proteins are not even expressed there in the first place. But the cancerous state of the prostate is acutely reliant on NSD2 and NSD1.” This specificity holds promise for developing therapies that minimize side effects.
In preclinical models, the drug showed impressive efficacy, particularly in androgen receptor-positive (AR+) prostate cancer cells, the most common type of prostate tumor. The researchers are now working to refine the drug, making it more suitable for human use.
While the current study focuses primarily on AR+ prostate cancer, the potential implications of targeting NSD2 and NSD1 extend beyond this subtype. The team’s screening of 120 cell lines from 22 different tumor types revealed that other cancers might also rely on NSD2 and NSD1 for their growth. This raises the possibility that drugs targeting these proteins could have broader applications.
The next step for the research team includes testing their drug candidate in mouse models. They also plan to investigate the biological mechanisms further, including how NSD2 might drive metastatic spread in prostate cancer. As Parolia emphasized, “We want to show that once we form these tumors, if we inactivate NSD2 or over-express it, we are able to drive these aggressive features of distant seeding, of metastatic spread, of invasion.”
At the same time, the researchers are working to improve the drug’s properties, making it more suitable for clinical trials. The ultimate goal is to combine NSD2/NSD1-targeting agents with existing FDA-approved androgen receptor antagonists, which could lead to synergistic effects and better patient outcomes.





