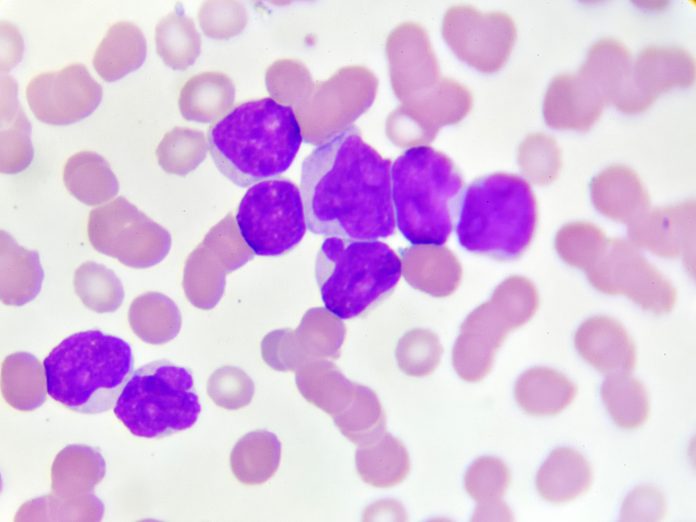
The U.S. National Institutes of Health has launched a unique portfolio of biomarker-driven precision medicine clinical trials, known as myeloMATCH, that will test new treatments for patients with myeloid cancers.
The patients will be enrolled in the trial from diagnosis through multiple stages of their treatment journey.
“MyeloMATCH provides a portfolio of biomarker-driven treatment trials that adult patients newly diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) will enroll to sequentially over their entire treatment journey,” said co-chair of myeloMATCH’s senior science council Harry Erba, MD, PhD of Duke University School of Medicine. “At each step along that journey, the goal is to continually reduce the patient’s tumor burden, to target residual disease more effectively, and ultimately cure more patients of the disease.”
Richard Little, MD, of the National Cancer Institute’s (NCI) Division of Cancer Treatment and Diagnosis and NCI coordinator for myeloMATCH, added that “having this library of genomic findings throughout the treatment journey will provide valuable information on clonal evolution for the tumors and provide opportunities for us to learn more about treatment sensitivity, resistance, and the opportunity to better control the disease. I don’t think that that this strategy has been done in any other setting.”
MyeloMATCH, which stands for Myeloid Malignancies Molecular Analysis for Therapy Choice, aims to recruit more than 5000 patients with newly diagnosed with AML or MDS. Each patient is initially enrolled in the myeloMATCH master screening and reassessment protocol during which they undergo rapid genetic testing of their tumor samples. Samples are screened using the FDA-approved Ion Torrent Genexus platform, which generates results within 72 hours.
“This is a huge improvement in previous turnaround times,” said Gail Sperling, MPH, lead patient advocate on the myeloMATCH senior science council.
Patients will then be matched to a substudy testing a treatment appropriate for the specific genetic changes and characteristics associated with their disease, if one is available, or to a standard-of-care option (known as the Tier Advancement Pathway) if an appropriate substudy is not available. Patients in the Tier Advancement Pathway can later have their biomarkers tested again and may be able to join a genetically matched myeloMATCH trial at a later stage of treatment.
The myeloMATCH trials, which are primarily phase II studies, are organized into four “tiers” according to the stage of the patient’s cancer treatment journey they address.
- Tier 1 trials offer initial induction therapy for newly diagnosed patients.
- Tier 2 trials treat patients for residual disease after initial therapy.
- Tier 3 trials offer consolidation therapy or transplant.
- Tier 4 trials treat progressively lower levels of residual disease burden that may remain.
As an enrolled patient completes a course of treatment, new specimens will be collected and sent for genetic testing with increasingly sensitive tools, such as next-generation sequencing, to identify ultra low-level measurable residual disease. If that testing shows the patient’s disease has been significantly reduced, a patient may be assigned to a new trial in a later tier.
“Ultimately, we hope to have patients who have completed all of their therapy but may still have residual disease that would be responsible for a relapse, and we hope to be able to identify what that is and target it, and the test will be by using such sensitive assays and potentially targeting residual disease, can we better control and forestall relapse, or even cure at the same time,” said Little.
So far, there are 143 clinical sites registered with the trial and over 80 patients have been screened within the master screening trial, noted Little. Three treatment trials are active for patients with AML, with one additional study undergoing final approval that is due to be activated in the next week or so. A further 14 substudies are under development in tiers one through three, and there are currently over 20 pharma and biotech partnerships with NCI to conduct myeloMATCH.
“MyeloMATCH is a fantastic opportunity to bring the advances of drug development, genetics, and diagnostics to large numbers of patients with AML or MDS. What we learn from myeloMATCH may have a major impact on the future of clinical trials in leukemia and beyond,” said is study chair for the core MYELOMATCH screening protocol Jerald Radich, MD, from the Fred Hutch Cancer Center and the SWOG Cancer Research Network.
MyeloMATCH’s senior science council co-chair Mark Litzow, from the Mayo Clinic, added: “The increasing understanding of the genetic heterogeneity of these diseases and the development of treatments that target these genetic abnormalities has brought us to this opportunity to more precisely and effectively treat these disorders in a comprehensive manner that focuses on care from diagnosis to cure.”
MyeloMATCH is being conducted by the National Clinical Trials Network, with the participation of the NCI Community Oncology Research Program. Initial substudies will be led by the SWOG Cancer Research Network, the Alliance for Clinical Trials in Oncology, the ECOG-ACRIN Cancer Research Group, and the Canadian Cancer Trials Group. The Frederick National Laboratory for Cancer Research, Fred Hutch Cancer Center, and Children’s Hospital Los Angeles will provide clinical laboratory support for the substudies.





