Researchers from the Medical Research Council Laboratory of Molecular Biology (MRC LMB) in Cambridge, England and the UK Dementia Research Institute (UK DRI) at the University of Cambridge have developed new potential therapies that selectively remove the aggregated tau tangles to treat Alzheimer’s disease (AD). Their work, detailed in two separate papers published in Cell and Science, suggests that these new therapies could not only treat Alzheimer’s but also other neurodegenerative diseases characterized by protein aggregation, such as motor neurone disease, Huntington’s disease, and Parkinson’s disease.
The new therapies leverage a protein known as TRIM21, which has been re-engineered to selectively remove tau aggregates while preserving healthy tau proteins. “Tau aggregates are tucked away inside brain cells and very difficult to degrade,” said Will McEwan, PhD, co-leader of the studies from the UK Dementia Research Institute. “Critically, these new TRIM21-based therapies can be delivered directly inside cells, where the majority of tau aggregates reside.”
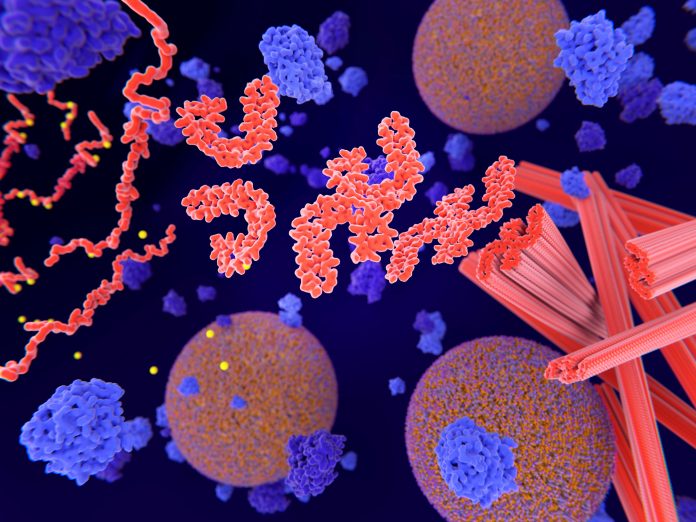
Tau tangles, which form inside nerve cells, are closely linked with cognitive decline in Alzheimer’s disease. This is in contrast to amyloid plaques, which accumulate between brain cells and are the target of existing antibody therapies. While antibody treatments can address amyloid plaques, they face challenges in penetrating cells to address tau tangles.
Current approaches to tackling tau inside cells include antisense oligonucleotides (ASOs), which aim to reduce tau levels. However, ASOs are not selective and can also eliminate healthy tau proteins, potentially leading to unknown long-term side effects. Healthy tau plays a critical role in maintaining the structural integrity of nerve cells.
The new TRIM21-based therapies aim to overcome these limitations. TRIM21, a protein involved in the immune response to viruses, was first identified in the lab of Leo James, PhD, at the MRC Laboratory of Molecular Biology. The researchers repurposed TRIM21 to target tau aggregates by switching out antibodies that bind viruses for antibodies that bind to tau. This method ensures that only the disease-linked tau is removed while preserving the healthy tau.
In their studies, the team developed two distinct therapies. The first, known as “RING-nanobody,” combines a tau-binding nanobody with the TRIM21 RING. The second, “RING-Bait,” has the TRIM21 RING joined to a copy of the tau protein itself. The RING-tau protein acts as bait—the aggregate incorporate and the TRIM21 RING as well. Once multiple RING-Baits are added to the aggregate, they become activated and destroy the entire aggregate.
When tested inside cell models containing aggregated tau, both TRIM21 therapies cleared the tangles, while leaving healthy tau intact.
“Neurodegenerative diseases can have tau proteins that misfold in many different ways, raising the possibility of needing a different treatment for every disease. A useful aspect of RING-Bait is because it is attached to a tau protein, it’s a universal Trojan horse that should be incorporated into different types of tau aggregates,” said study co-leader James in touting the potential of this new approach.
The efficacy of these therapies was tested in mice with tau aggregates and delivery of the therapies was via adeno-associated virus (AAV). Mice treated with the new therapies showed significant reductions in tau tangles in the brain and showed improved motor functions, as assessed by an AI program that measured how well the mice ran.
“It was unknown whether specifically removing tau aggregates inside the cell would be enough to halt the progression of disease, said Lauren Miller, PhD, of the UK Dementia Research Institute and one of the study’s authors. “It is encouraging that a RING-Bait approach reduces disease severity in our model systems, as this suggests that the selective removal of tau aggregates is a valid therapeutic approach. Further work will be needed to demonstrate this beneficial effect is found across multiple models of human disease.”
The researchers caution that while these therapies show promise in animal models, significant development is needed before human trials can begin. The challenge includes developing safe and effective methods for delivering these therapies to the human brain.





