New research from Julio Aguirre-Ghiso, PhD, and colleagues at the Albert Einstein College of Medicine has uncovered insights into how the immune system can suppress metastatic growth in the lungs. The findings center around the role of alveolar macrophages (AMs), specialized immune cells residing in the lung’s airspaces, in keeping disseminated cancer cells (DCCs) dormant. This discovery not only advances our understanding of metastasis prevention but also opens potential avenues for developing novel cancer therapies. Their paper is published in Cell.
Early disseminated cancer cells and dormancy
Disseminated cancer cells (DCCs) can remain dormant for extended periods—sometimes years or even decades—before reactivating and proliferating into full-blown metastases. “What we discovered is that early-stage breast cancer cells can spread to the lungs and remain dormant, interacting with immune cells in a way that prevents them from growing into tumors,” Aguirre-Ghiso explained.
The study focuses on HER2+ breast cancer, a subtype known for its aggressiveness and potential for early dissemination. While previous research has identified genetic and molecular factors responsible for the dormancy of these cells, what remained unclear was how dormancy could be sustained for such long periods. The team identified alveolar macrophages as key players in this process, revealing an interaction between DCCs and these immune cells that prevents cancer from progressing.
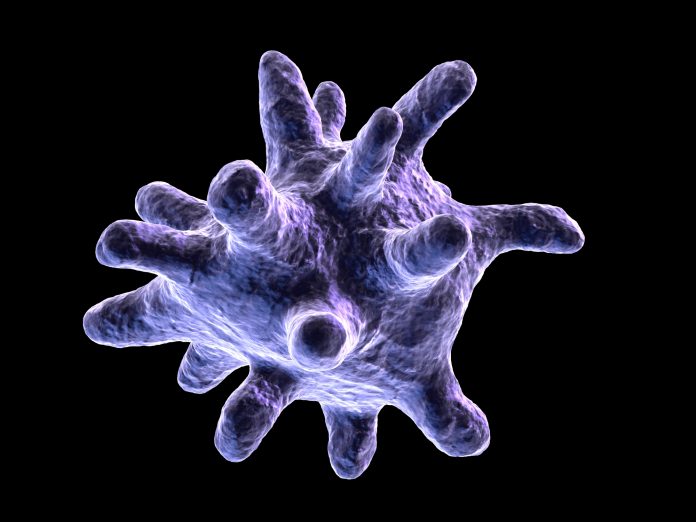
Alveolar macrophages: Guardians of dormancy
Alveolar macrophages are critical to lung health, regulating tissue homeostasis, immune responses, and clearing debris from airspaces. Their role in cancer dormancy, however, had not been explored in detail until now. Aguirre-Ghiso’s team used imaging techniques, including live microscopy, to observe how these macrophages interact with DCCs in real-time. “We discovered, kind of surprisingly, that when the cancer cells are kept dormant, they are persistently interacting with the macrophages,” he said. These intimate, long-term interactions between the two cell types appear crucial for maintaining cancer dormancy.
The research team demonstrated that alveolar macrophages induce dormancy in DCCs through signaling mechanisms. Specifically, they found that the transforming growth factor-beta 2 (TGF-β2) produced by the macrophages acts on cancer cells via a receptor called TGF-βRIII. This signaling pathway prevents the cancer cells from dividing and forming metastases. However, once this pathway is disrupted, either by genetic manipulation or the depletion of macrophages, dormant DCCs can “awaken” and initiate metastatic growth.
A critical balance: Dormancy vs. reactivation
One of the key findings from the study is the vulnerability of the dormancy mechanism. By depleting alveolar macrophages in their mouse models, the researchers saw a dramatic shift: dormant DCCs began to proliferate, leading to metastasis in 50% of the mice. “The loss of alveolar macrophages removes this protective mechanism and allows the cancer cells to start dividing again,” Aguirre-Ghiso noted. This observation underscores how critical these immune cells are in maintaining dormancy and preventing metastatic growth.
Interestingly, the study also found that the cancer cells themselves can adapt to escape dormancy. Advanced, more aggressive cancer cells are able to “turn off” the receptors that respond to the macrophages’ dormancy-inducing signals. “Essentially, the cancer cells shut down the antennas that allow them to hear the signals from the macrophages,” added Aguirre-Ghiso. This allows the cancer cells to become resistant to the macrophages’ suppressive influence and to proliferate, leading to metastatic lesions.
The study’s findings hold promise for future cancer therapies aimed at preventing or delaying metastasis. One possible avenue is the manipulation of macrophages themselves to maintain their dormancy-inducing functions. “Now we have a sense of what molecules may need to be turned on in the macrophages to keep them suppressing cancer cell growth,” said Aguirre-Ghiso. This could involve developing drugs that enhance the macrophages’ ability to produce TGF-β2 or maintaining their “patrolling” behavior over cancer cells.
Another potential approach is to engineer alveolar macrophages to continuously produce the molecules that suppress cancer growth. Such cell-based therapies, though still in early stages of development, could become a powerful tool in preventing metastatic recurrence. “We’re considering ways to engineer the macrophages so they always make the molecules that prevent cancer cells from growing. This could be a kind of cell therapy for patients,” Aguirre-Ghiso explained.
Despite these promising findings, the researchers explain future challenges. Cancer cells, particularly those from more advanced tumors, have the ability to evade the macrophages’ influence. Additionally, once metastases start to form, macrophages themselves seem to undergo a transformation, shifting from anti-metastatic to pro-inflammatory roles that may support tumor growth. Understanding and reversing this shift will be key to developing therapies that maintain the macrophages’ protective role over time.
As Aguirre-Ghiso put it, “The more aggressive cancers actually turn off the mechanism of recognition and response to macrophages. So, part of the challenge is figuring out how to re-establish or sustain that dormancy, especially in more advanced cases.”





