An international study, led by researchers at the Massachusetts General Hospital, has found that a combination of anti-CXCR4 and anti-PD1 therapies can improve treatment outcomes for hepatocellular carcinoma (HCC), the most common form of liver cancer. While immunotherapy has shown significant improvements in treating certain cancers, its effectiveness against HCC has remained limited due to the development of treatment resistance often from the lack of dendritic cells. This new approach, published in the journal Cancer Immunology Research, details a method to address this obstacle by increasing the activity of dendritic cells to significantly improve immune response.
“Our previous reports have focused on the tumor microenvironment in liver cancer, including the role of CXCR4, a receptor for CXCL12, which helps weaken the immune system’s ability to fight cancer, making it easier for the tumor to grow and spread,” said Dan G. Duda, DMD, PhD, senior author of the study and director of translational research in gastrointestinal radiation oncology at Massachusetts General Hospital. “However, CXCR4 inhibition alone has been largely ineffective across multiple cancer models, suggesting that CXCR4 targeting should be tested in combination with other strategies.”
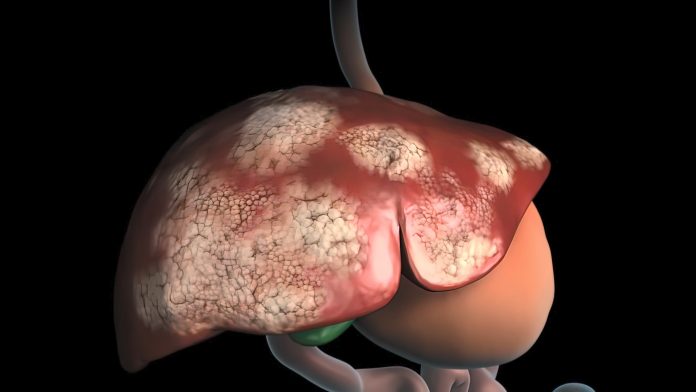
Liver cancer, a leading cause of cancer-related deaths worldwide, and the fifth leading cause of cancer deaths in the U.S., has long been resistant to many forms of treatment. Despite the introduction of immunotherapy, which has shown some benefits, most patients with advanced liver cancer still experience poor outcomes, due to it being a “cold” cancer that lacks the necessary immune cells in the tumor microenvironment to mount an effective attack against tumors. Despite these challenges, recent studies have shown that combination therapies that inhibit angiogenesis in combination with immunotherapy have shown greater efficacy than the kinase inhibitor sorafenib, the long-standing standard of care for HCC. Still, these approaches showed limited improvement as virtually all patients in previous studies experienced a cancer recurrence.
In this preclinical study, the investigators tested the combination of anti-CXCR4 and anti-PD1 therapies in mouse models, to determine if this approach could overcome the limitations of CXCR4 inhibition alone. While CXCR4 antagonists like AMD3100 have been tested in the past, they have shown limited effectiveness due to issues like a short half-life and a lack of specificity. The new study used a combination of long-acting antibodies targeting CXCR4, which proved more effective in reprogramming the “cold” liver tumor environment into one more conducive to immune response.
The results were promising. The combination therapy increased the presence of dendritic cells, which are a key to initiating an immune response. Activated dendritic cells help guide other immune cells, such as CD8+ T cells, to the tumor site.
“We discovered the potential of anti-CXCR4 to reprogram the immunologically ‘cold’ microenvironment of liver cancer to an immunologically ‘hot’ one because of its effects on dendritic cells and the benefits when combining them with anti-PD1, a current standard therapy for patients with liver cancer.”
Additional research revealed that the anti-CXCR4 treatment not only promoted dendritic cell activation but also enhanced the ability of these cells to produce chemokines that attract more immune cells into the tumor. This synergy between anti-CXCR4 and anti-PD1 therapy resulted in better anti-cancer responses compared to anti-PD1 therapy alone.
“Our study demonstrates that combining anti-CXCR4 and anti-PD1 is more effective than anti-PD1 alone in mouse models of liver cancer, and that the increased dendritic cell activity contributes to the effectiveness of this combination therapy,” Duda added.
These findings are potentially a significant step to advancing more effective treatments for HCC, which currently has limited therapeutic options.
The next step will be to evaluate the combination therapy’s safety and efficacy in humans, with a Phase I clinical trial to led by Ilyas Sahin, MD, currently being planned at Mass General.





