A protein that can trigger the loss of immune regulation and multiple sclerosis (MS) has been identified by a team at Yale School of Medicine and collaborators. PRDM1-S is involved in immune function. Through its effects on regulatory T cells, upregulation of PRDM-S leads to “a dynamic interaction of multiple genetic and environmental factors, including high salt uptake,” according to the team’s press release.
“These experiments reveal a key underlying mechanism for the loss of immune regulation in MS and likely other autoimmune diseases,” said David A. Hafler, senior author of the paper and chair of Yale’s department of neurology. “They also add mechanistic insight into how Treg [regulatory T cell] dysfunction occurs in human autoimmune diseases.”
The researchers say their findings, published in the journal Science Translational Medicine, also reveal a new target for a universal treatment for human autoimmune disease. The work was led by Hafler and Tomokazu Sumida, an assistant professor at Yale School of Medicine.
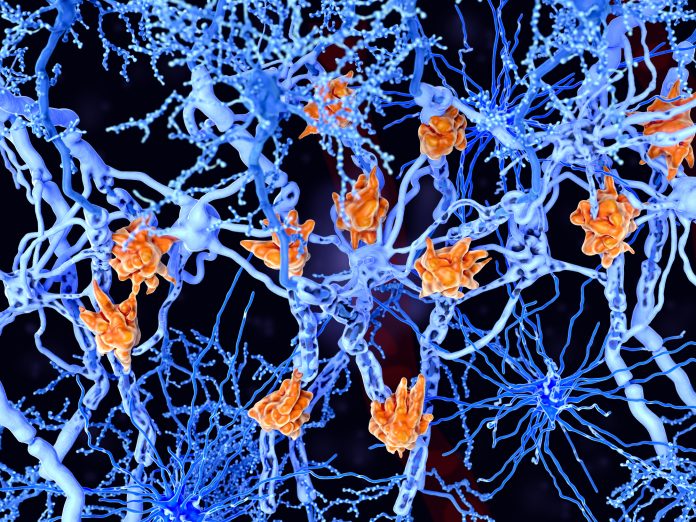
In earlier research, Hafler’s lab discovered regulatory T cells, which can suppress the human immune system. They later found that when defective, these cells are an underlying cause of MS. However, the mechanism behind this dysfunction has long remained unclear.
Autoimmune diseases, among the most common disorders of young adults, are known to be affected by genetic and environmental factors, including vitamin D deficiency and fatty acids. In another earlier study, Sumida and Hafler found that high levels of salt also contribute to the development of multiple sclerosis, an autoimmune disease of the central nervous system.
Specifically, they saw that high salt induces inflammation in a type of CD4 T cells, while also causing a loss of regulatory T cell function. This, they found, is mediated by a salt-sensitive kinase, or enzyme critical for cell signaling, known as SGK-1.
For the new study, researchers used RNA sequencing to compare gene expression in patients with MS to that of expression in healthy individuals. In patients with MS, the researchers saw increased expression of PRDM1-S (primate-specific transcription factor), also known as BLIMP-1, which is involved in regulating immune function.
Surprisingly, PRDM1-S induced increased expression of the salt-sensitive SGK-1 enzyme, leading to disruption of regulatory T cells, the researchers found. Moreover, they found similar overexpression of PRDM1-S in other autoimmune diseases, suggesting that it may be a common feature of regulatory T cell dysfunction.
“Based on these insights, we are now developing drugs that can target and decrease expression of PRDM1-S in regulatory T cells,” Sumida said. “And we have initiated collaborations with other Yale researchers using novel computational methods to increase the function of regulatory T cells to develop new approaches that will work across human autoimmune diseases.”
The study was done with Bradley Bernstein and Manolis Kellis, longtime collaborators of Hafler from the Broad Institute of MIT and Harvard, and several other research institutions.





