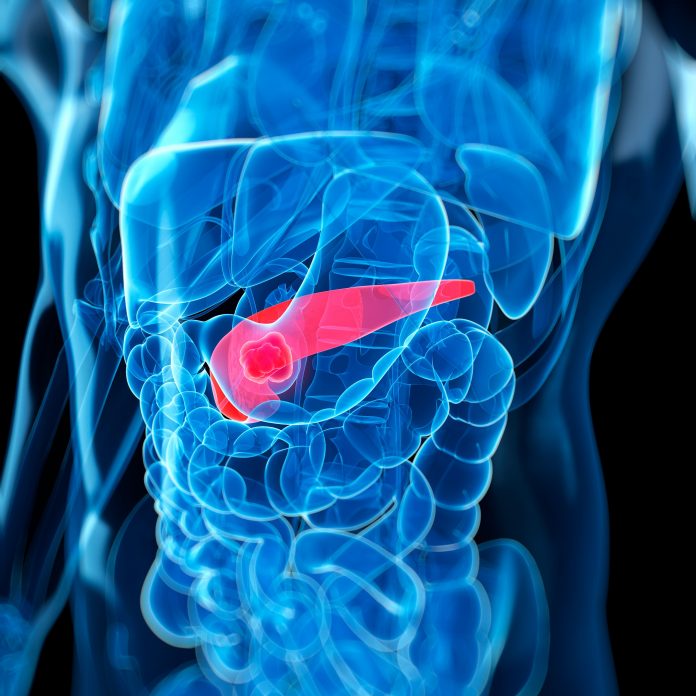
Researchers at the Mayo Clinic Comprehensive Cancer Center have shown that the presence of mutant KRAS (mKRAS) circulating tumor DNA (ctDNA) in plasma and peritoneal fluid is associated with an increased risk for metastases and death in patients with pancreatic ductal adenocarcinoma (PDAC).
Senior study author Mark Truty, MD, hepatobiliary and pancreatic surgical oncologist within Mayo Clinic’s Department of Surgery, said that the findings are “a major advancement for pancreatic ductal adenocarcinoma.”
He explained that although ctDNA blood testing is performed at most major cancer centers on a variety of commercial platforms, the prognostic significance of the findings is often unclear.
“Our data suggests that a positive test indicates a high likelihood of metastatic disease in patients whose imaging does not show any metastases,” Truty told Inside Precision Medicine. This information can significantly impact treatment decisions, particularly among patients for whom an aggressive surgical approach is being considered.
Such patients “may require extended neoadjuvant chemotherapy and be counseled on the predicted utility or futility of subsequent surgery in the absence of obvious metastatic progression during neoadjuvant therapy,” Truty and co-authors wrote in the Annals of Surgical Oncology.
Truty and team used a droplet digital PCR method, developed at the Mayo Clinic and approved for clinical use in 2018, to measure mKRAS ctDNA in the plasma and/or peritoneal fluid of 785 patients with non-metastatic PDAC between 2018 and 2022.
They focused on mKRAS because the mutations are rarely found in non-cancerous cells but are present in almost 90% of PDAC tumors.
Of the 743 patients who underwent baseline plasma ctDNA mKRAS testing, 104 (14%) were mKRAS-positive. These patients were significantly more likely than their mKRAS-negative counterparts to experience early postoperative recurrence or death within six months of resection (46% vs 13%).
They also had a significantly higher rate of subsequent metastatic disease (78% vs 49%) during a median 16 months of follow-up. The metastases were more likely to be derived from the blood (hematogenous) than the peritoneal fluid (78% vs 62%).
In addition, plasma mKRAS-positive patients were significantly less likely to be alive at follow-up than mKRAS-negative patients (20% vs 58%). Median overall survival (OS) was 13.3 months for plasma mKRAS-positive patients compared with 26.9 months for patients who were plasma mKRAS-negative, and further analysis showed that positive plasma mKRAS status was independently associated with a significant 2.24-fold increased risk for death.
Positive mKRAS results on peritoneal samples were also associated with worse outcomes. In this case, 29% of 419 patients who underwent baseline peritoneal fluid mKRAS testing had a positive result. They were significantly more likely to have metastatic disease at follow-up than peritoneal mKRAS-negative patients (67% vs 42%) but the metastases were more likely to be peritoneal than hematogenous (58% vs 26%).
Furthermore, peritoneal mKRAS-positive patients were significantly less likely to be alive at follow-up than mKRAS-negative patients (56% vs 67%), with median OS at 20.8 and 27.9 months, respectively.
Among patients who underwent both plasma and peritoneal mKRAS testing (n=377), those who were positive for mKRAS ctDNA in both samples (n=10) had the worst median OS, at 10 months, followed by patients who were plasma positive/peritoneal negative (n=26; 15 months) and those who were plasma negative/peritoneal positive (n=92; 27 months). Patients negative in both samples (n=244) had the longest median OS, at 28 months.
Truty said that “for patients being considered for local treatment (i.e., surgery and/or radiation) both tests are needed to understand the risk of metastatic disease. Surgery/radiation is not beneficial in patients with metastatic disease in general and thus having an understanding and accurate staging at diagnosis is critical for treatment decisions.”
The study also showed that the levels of both plasma and peritoneal mKRAS ctDNA correlated with the risk for metastatic disease and death, with higher levels associated with a greater risk.
In addition, the blood test could be used to monitor treatment response. In a small subgroup of 82 patients who underwent repeat plasma mKRAS testing, 32 patients were initially positive and 29 (91%) of those patients turned negative on repeat testing after receiving neoadjuvant chemotherapy.
Survival analysis showed that patients who remained positive on repeat testing had a median survival of just seven months compared with 17.5 months for patients who were initially positive but turned negative. Patients who remained negative on repeat testing had the best OS at 32 months.
Truty noted that there are currently multiple clinical trials looking at multi- or mutation-specific KRAS inhibitors that could be used to treat patients with PDAC who are mKRAS positive. He said that the mKRAS ctDNA testing could be used to enrich patient populations for future use with these new agents.








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




