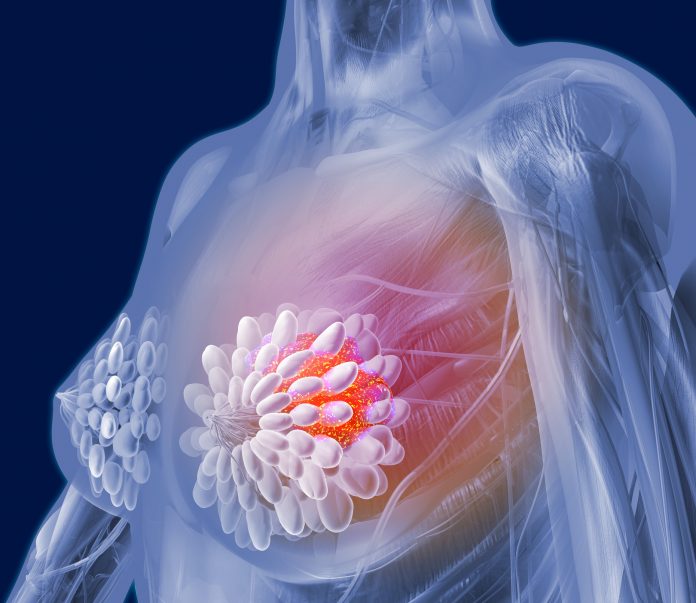
Researchers from the University of Texas MD Anderson Cancer Center report that women who do not undergo breast surgery after a complete response to neoadjuvant systemic therapy (NST) have excellent outcomes at five years, with no recurrences seen, suggesting that selective avoidance of surgery may be a possibility.
Lead author Henry Kuerer, MD, PhD, professor of surgery and executive director breast programs at MD Anderson, told Inside Precision Medicine that the findings represent a “new paradigm for the management of select patients with HER2-positive and triple-negative breast cancers.”
Approximately 60% of patients with these cancers will have a pathologic complete response (pCR) to NST, indicating an excellent long-term prognosis. This high pCR rate has raised questions regarding the necessity of breast surgery for patients without residual disease after NST.
In the first study of its kind, 50 women aged 40 years or older (median age 62 years) with HER2-positive (58%) or triple-negative (42%) invasive breast cancer who had residual breast lesions of less than 2 cm after NST underwent image-guided vacuum-assisted biopsy (VAB) with a minimum of 12 cores obtained via a 9G needle.
The VAB technique was developed at MD Anderson by Kuerer and colleagues. In early studies, they showed that they could precisely biopsy the region where the cancer had shrunk to less than 2 cm. “Utilizing this technique, the false-negative rate was less than 5%, with an accuracy of 98%,” he noted.
The biopsies were examined histologically for any residual abnormalities and 31 (62%) patients had a pCR, i.e., no invasive or in situ disease, including eight patients with initial nodal metastases who had an axillary pCR confirmed after targeted axillary node dissection.
These patients underwent whole-breast radiotherapy with a boost but did not have breast surgery. They were then monitored with physical examinations and mammography every six months. The remaining 19 patients with residual cancer detected on VAB had standard breast and axillary surgery.
The researchers report in JAMA Oncology that at a median follow-up of 55.4 months, none of the 31 patients who avoided surgery had experienced ipsilateral breast tumor recurrence, and the disease-free and overall survival rates were both 100% for these patients.
The standard practice for invasive breast cancer is surgical management, so all of the 31 patients would have undergone surgery if they had not been involved in the trial. Yet, Kuerer was not surprised back the lack of recurrence.
“There was no guesswork with this new paradigm for the management of meticulously selected patients after neoadjuvant systemic therapy,” he said. “We followed these patients extremely closely at six-month intervals with imaging and physical examinations and were delighted that none of the patients had a recurrence, as we had already predicted, since no residual breast cancer was noted on the needle biopsy.”
The researchers also investigated how the women felt about participating in the trial. At baseline, the participants reported relatively high levels of comfort with their decision to take part and forego breast surgery, with a mean baseline Decisional Regret Scale score of 15.2 out of 100. By five years, this had fallen significantly to a score of 2.5, showing that decisional comfort increased with time. Overall health-related quality of life, including physical, social/family, emotional, functional, and breast cancer–specific well-being also all improved significantly during follow-up.
“I think that most patients would prefer avoiding therapies that are not essential for their well-being and preventing complications such as pain syndrome, swelling of the arm, infection, adverse cosmetic outcomes, and even, for some patients, psychological trauma from breast cancer surgery,” said Kuerer.
However, he stressed the importance of further clinical trials before surgical omission can become standard in select patients and emphasized the need for strict eligibility criteria and technical protocols.
“I think it is essential that VAB is the only biopsy method at this time to utilize all the criteria we established in our foundational trials to select patients safely,” Kuerer remarked. “There have been other biopsy trials looking at the accuracy in determining a pathological complete response, but they did not ensure technical accuracy, used a needle size that was too small without appropriately sampling the residual region, and did not include the extensive microscopic evaluation of the small portions of tissue to ensure no carcinoma cells.”
The researchers have now expanded the clinical trial to include a total of 100 patients at MD Anderson Cancer Center, and the protocol is also being investigated in South Korea in the Optimist study, which is currently accruing patients.








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




