Researchers from The University of Texas MD Anderson Cancer Center have shown that mutations in the STK11 and/or KEAP1 tumor suppressor genes could serve as biomarkers for identifying lung cancer patients likely to benefit from dual immune checkpoint blockade.
The study, published in Nature “advances precision medicine for a substantial fraction of patients with advanced non-squamous NSCLC [non-small-cell lung cancer],” said co-lead author Ferdinandos Skoulidis, MD, PhD, associate professor of thoracic/head and neck medical oncology at The University of Texas MD Anderson Cancer Center.
He explained that although it is well-known that patients with STK11 and KEAP1-mutated NSCLC exhibit primary resistance to treatment with PD-1 or PD-L1 immune checkpoint inhibitors, how best to treat them “has remained a clinical conundrum,” he said. “The main motivation for this study was to determine the best therapeutic approach for this PD-(L)1 inhibitor-recalcitrant group of patients with a major unmet clinical need.”
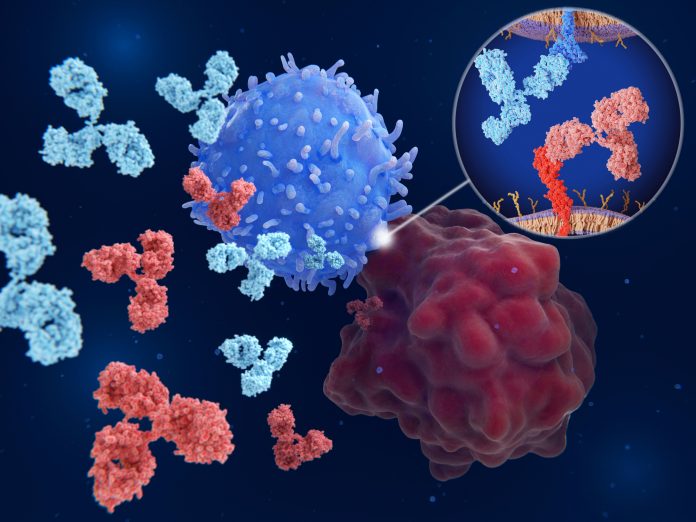
Previous studies have shown that dual immune checkpoint blockade with a PD-(L)1 inhibitor plus a CTLA4 inhibitor is associated with higher rates of anti-tumor activity in NSCLC when compared with PD-(L)1 inhibitors alone, but there are currently no validated biomarkers to identify which patients will benefit from dual ICB.
To address this, Skoulidis and team first analyzed data from multicenter cohort of 871 patients with advanced non-squamous NSCLC who were treated with standard chemo- therapy (carboplatin or cisplatin plus pemetrexed) or with chemotherapy plus the PD-1 inhibitor pembrolizumab.
They found that, among the patients given pembrolizumab, those with STK11 or KEAP1 mutations had significantly shorter progression-free survival (PFS) and overall survival (OS) than those who had wild-type tumors. In addition, the combination of the two alterations resulted in a worse response to pembrolizumab than did either the STK11 or KEAP1 alterations alone, at objective response rates (ORRs) of 7.1% versus 29.6% and 28.6%, respectively. By comparison, the ORR was 48.6% among patients with neither mutation.
To further investigate the mechanisms that might underlie the resistance of STK11 and KEAP1 mutated tumors to PD-(L)1 inhibitors, the team studied the immune and genetic characteristics of tumors from 8592 patients with non-squamous NSCLC. In all, 25.2% of patients had an STK11 and/or KEAP1 mutation with the proportion increasing to 32.4% among individuals whose tumors also harbored a KRAS mutation.
The analysis showed that mutations in the STK11 and KEAP1 genes were linked to a less favorable tumor environment, often referred to as a “cold” microenvironment. This type of environment had many suppressive myeloid cells and fewer CD8+ cytotoxic T cells, which are important for fighting tumors. However, the investigators noted that CD4+ immune cells were less impacted and remained present in tumors with STK11 and/or KEAP1 mutations.
Based on these observations, Skoulidis and colleagues hypothesized that dual checkpoint inhibitors, targeting CTLA4 in addition to PD-1 or PD-L1, may improve outcomes. They therefore evaluated data from 1013 patients with metastatic NSCLC who took part in the phase III POSIEDON study, which compared standard-of-care chemotherapy alone with chemotherapy plus the PD-L1 inhibitor durvalumab or with the combination of durvalumab and the CTLA4 inhibitor tremelimumab.
They found that, in line with previous observations, patients with STK11 and KEAP1 mutations had significantly worse OS and PFS in the chemotherapy plus durvalumab arm than those with wild-type tumors given the same treatment.
“This indicates that patients with STK11 and/or KEAP1 mutations derive little, if any, benefit from the addition of durvalumab to chemotherapy and that the benefit of [chemotherapy plus durvalumab] is largely confined to patients who lack mutations in either gene,” the authors write.
However, they also found that the addition of tremelimumab mitigated the resistance to chemotherapy plus durvalumab among the patients with STK11 and/or KEAP1 mutations, and that this group may derive greater benefit from CTLA4 inhibition than do patients who lack either alteration.
For example, in the STK11/KEAP1 mutated subgroup, the ORR was higher in the dual immune checkpoint blockade arm (42.9%) than in the chemotherapy plus durvalumab (30.2%) or chemotherapy only (28.0%) arms.
Moreover, median OS was more than doubled when tremelimumab was added to durvalumab and chemotherapy (15.8 versus 7.3 months), whereas little benefit was observed from the addition of tremelimumab in the group lacking mutations in both genes (17.2 versus 17.1 months).
“These findings support that NSCLC patients with STK11 or KEAP1 mutations are relatively resistant to standard combinations of PD-(L)1 inhibitors and chemotherapy but can benefit markedly when a CTLA-4 inhibitor is added to their treatment regimen,” said co-lead author John Heymach, MD, PhD, chair of thoracic/head and neck medical oncology at The University of Texas MD Anderson Cancer Center. “We are optimistic that these results will prompt clinicians to consider this novel therapeutic approach as a preferred treatment option.”
The study also “provides important insights into mechanisms and immune cell subsets that mediate the observed benefit from the addition of CTLA-4 inhibitors,” added Skoulidis.





