New research to be presented at this year’s Annual Meeting of the European Association for the Study of Diabetes (EASD) in Hamburg, Germany (2-6 October) and published in the journal Diabetes Therapy suggests that the diagnosis threshold for type 2 diabetes (T2D) should be lowered in women aged under 50 years, since natural blood loss through menstruation could be affecting their blood sugar management. The study is by Dr Adrian Heald, Salford Royal Hospital, UK, and colleagues.
Analysis of the national diabetes audit results has shown that women of younger age with type 2 diabetes mellitus (T2D) seem to have a higher mortality rate than men. The underlying mechanisms remain unclear. However, it is known that women are on average diagnosed with T2D at a later age than men. In this new study, the authors investigated whether a contributing factor to this late diagnosis may be a sex difference in the levels of glycated hemoglobin (HbA1c – a standard measure of blood sugar control) due to hemoglobin replacement linked to menstrual blood loss.
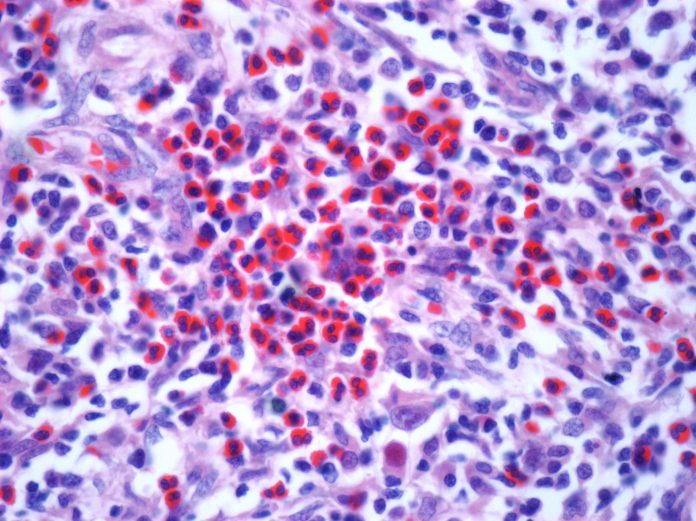
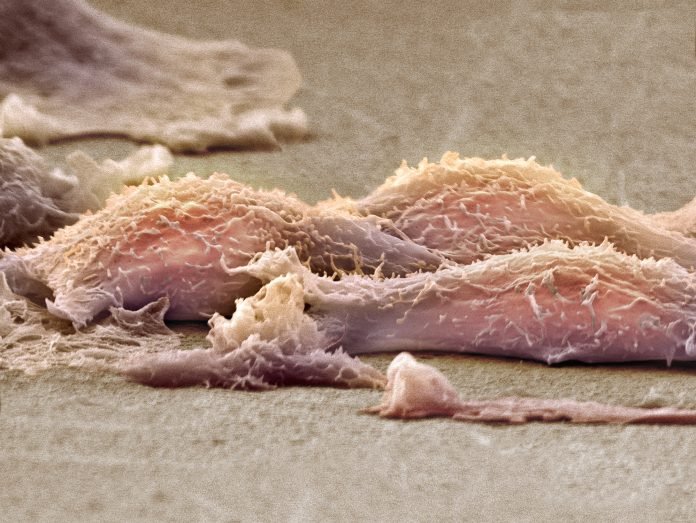
This mechanism behind this could be shorter erythrocyte (red blood cell) survival which results in shorter exposure of hemoglobin to glucose compared with individuals who do not menstruate. Given that the diagnosis of T2D is also based on HbA1c, the use of the same reference range irrespective of age and sex, when a slightly lower point for T2D for premenopausal women may be appropriate, could potentially lead to under diagnosis of T2D in women and missed opportunities for intervention.
The authors examined HbA1c testing across seven UK laboratory sites (representing 5% of UK population). They conducted an exploratory analysis in two cohorts: cohort 1 was from one laboratory tested between 2012 and 2019 (146,907 participants). They assessed the sex and age differences of HbA1c in individuals who underwent single testing only, that had not been diagnosed with diabetes and had an HbA1c result of equal to or less than 48 mmol/mol (the cut off for diagnosing diabetes). The process was replicated in cohort 2 results from six laboratories with individuals tested between 2019 and 2021 (total people included 938,678). The possible national impact was estimated by extrapolating findings based on the Office of National Statistics (ONS) England population data and National Diabetes Audit published T2D prevalence and related excess mortality.
At age 50 years, average HbA1c levels in women lag by approximately 5 years compared to men. The data also show women aged under 50 years old had an HbA1c distribution that was lower than that of men by an average of 1.6 mmol/mol (4.7% of the overall mean) while the difference in the distribution of HbA1c for individuals aged 50 years and over was less pronounced (See Figure B, full abstract). Further analysis showed that, at HbA1c of 48 mmol/mol, 50% fewer women could be diagnosed with T2D than men under the age of 50, whilst only 20% fewer women could be diagnosed with T2D than men over or equal to the age of 50. These findings were consistent with those in cohort 2.
Based on these observations, the authors estimated the effects of lowering the threshold for diagnosis of diabetes from HbA1c (48 mmol/mol) by 4.2% to 46 mmol/mol for women under the age of 50. This analysis showed that an additional 35,345 currently undiagnosed women in England would be reclassified as being diagnosed with T2D (17% more than the current 208,000 recorded women with T2D aged under 50 years). Lifestyle changes and treatment for diabetes would then be initiated for these women enabling improvement in health outcomes over both the short and longer term.
The authors also highlight that sex and gender differences in adverse cardiovascular risk factors are known to be present prior to the development of T2D. Once diagnosed, the prevalence of atherosclerotic cardiovascular disease is twice as high in patients with diabetes mellitus compared to those without diabetes mellitus. For women, diabetes mellitus is a stronger risk factor for cardiovascular disease than for men: women with diabetes aged 35–59 years have the highest relative cardiovascular death risk across all age and sex groups.
Furthermore, there is disparity in cardiovascular risk factor management between men and women, including in high-risk groups such as women with T2D. Women are less likely than men to receive treatment and cardiovascular risk reduction interventions that are recommended by international guidelines on diabetes. In addition, concordance with medication or prescription treating cardiovascular risk factors is lower in women than men with T2D, with less use of statins, aspirin and beta blockers. The authors say taken together, these factors mean “timely diagnosis of type 2 diabetes and initiation of preventative treatment has the potential to improve cardiovascular risk profile over lifetime and facilitate longer life quality and expectancy in women. Our findings provide evidence that the HbA1c threshold for this group should be re-evaluated.”
Source:
Journal reference:
Holland, D., et al. (2023). Is the Current Cut Point for Glycated Haemoglobin (HbA1c) Correct for Diagnosing Diabetes Mellitus in Premenopausal Women? Evidence to Inform Discussion. Diabetes Therapy. doi.org/10.1007/s13300-023-01482-6.