Here, we describe an isolated collagenoma in an HIV patient on long term ART. There has been one case in the literature describing eruptive collagenoma in an HIV patient [5]. However, causality in this case is questionable because eruptive collagenoma presented seven years prior to the diagnosis of HIV.
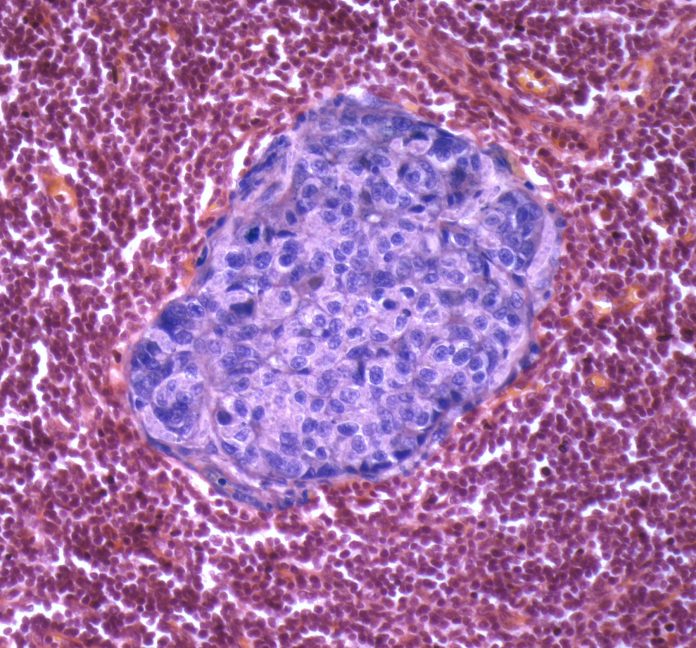
Histopathology of collagenomas shows thick and randomly arranged collagen bundles with diminished elastin and loss of normal empty spaces between bundles [6]. Special stains are not necessary to diagnose a collagenoma.
There are several differential diagnoses to consider when evaluating a painless subcutaneous, indurated nodule on the scalp in a patient of this age group, including lipoma, epidermal inclusion cyst, and pilar cyst. In a patient with HIV, it is important to consider HIV-associated lipodystrophy.
HIV has been classically associated with HIV-associated lipodystrophy and lipomas [4]. HIV infection can lead to increases in pro-inflammatory cytokines including TNF-alpha, IL-6, and IL-1beta. These cytokines can induce a stress response in adipocytes leading to lipodystrophy. Collagenomas, however, have not yet been reported in HIV patients. Collagen-producing fibroblasts are stimulated by IL-1, IL-10, and fibroblast growth factor. These cytokines are upregulated in HIV [7], which may play a role in the development of isolated collagenoma in our patient. More research is needed to determine the mechanism of the development of collagenoma in HIV patients.
ART medications can also cause lipodystrophy. Certain ART medications have a greater association with lipodystrophy in HIV patients, including protease inhibitors, zidovudine, didanosine, and stavudine [8]. The pathogenesis of lipodystrophy in HIV patients on ART is unclear but has been postulated to be due to metabolic abnormalities and inhibition of receptors involved in lipogenesis and lipolysis.
In addition to HIV-associated lipodystrophy and lipomas, HIV can also be associated with a host of other dermatologic conditions [9]. For example, due to impairment of the immune system, HIV patients have a greater risk of opportunistic skin infections, including deep fungal infections (e.g. cryptococcus, blastomycosis, histoplasmosis, and aspergillosis), viral infections (e.g. herpetic infections, molluscum contagiosum, and human papilloma viruses), and bacterial infections (e.g. cellulitis, syphilis, and bacillary angiomatosis). HIV is also associated with a higher risk of cutaneous malignancies such as Kaposi sarcoma, squamous cell carcinoma, basal cell carcinoma, and mycosis fungoides. Due to immune dysregulation, HIV patients are more likely to present with more severe inflammatory skin diseases as well, including psoriasis, seborrheic dermatitis, and atopic dermatitis.
Treatment options of collagenomas include surgical excision and intralesional corticosteroids [10]. There have been several reports of collagenomas treated by surgical excision resulting in complete resolution without recurrence. Cases of collagenomas treated with intralesional corticosteroids resulted in either substantial reduction in size or complete resolution [11, 12]. Attempts to treat collagenomas with cryotherapy have been largely unsuccessful [13].
We report an isolated collagenoma in an HIV patient. It is unclear if the pathophysiology of HIV or ART medications predispose patients to developing collagenomas. Collagenomas are rare, and further research is needed to elucidate the underlying mechanism of what might increase risk of collagenomas in HIV patients. It is important to keep collagenoma in the differential diagnosis when evaluating a patient with a large and indurated subcutaneous nodule.