
When it comes to studying and treating cancer, scientists and clinicians often think of applying two key areas of knowledge: the immune system and genomics. The combination of those fields—immunogenomics—is not quite a new field, but it is on the rise.
Even in 2015, Robert Holt, PhD, scientific co-director of the cancer immunotherapy program at the BC Cancer Research Institute in Vancouver, Canada, wrote that immunogenomics “is a broad and diversified field that has a long history.” He added that immunogenomics “is an information science.”
Today, scientists around the world apply immunogenomics to cancer. “Since the immune system is a central component in surveillance of the tumor and its development, immunogenomics analyses can provide insights into the status of the immune system in several ways,” said Hubert Hackl, PhD, assistant professor of bioinformatics and leader of the computational biology and immune-oncology research group at the Medical University of Innsbruck in Austria. “Information can be gained on the immune contexture in the tumor microenvironment, the interaction between immune cells and tumor cells such as immune checkpoints, chemokines, and cytokines, but also antigen presentation and activation of the adaptive immune system.” As he emphasized: “This could be crucial for therapy response, especially immunotherapy.”

Assistant Professor
Medical University of Innsbruck
BRCAness and ovarian cancer
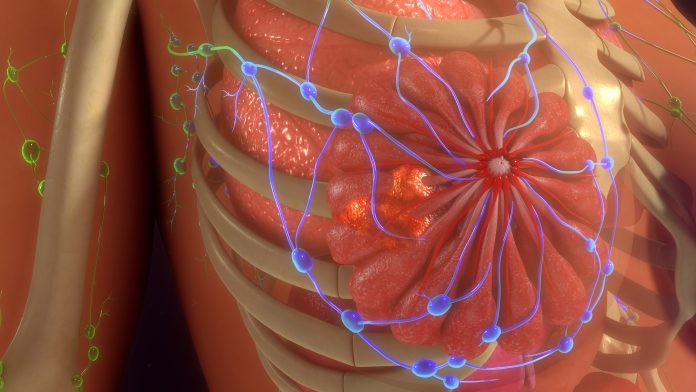
Mutations in BRCA genes are some of the most well-studied genomic modifications involved in cancer, especially breast cancer. The names of these genes are even an abbreviation—BReast CAncer—that suggests a role in one type of cancer, but mutations in BRCA genes can increase the risk of many other cancers, like ovarian, pancreatic, and prostate cancers.
For example, a mutation in the BRCA1 gene can cause homologous recombination deficiency, which is an error in the repair of breaks in double-stranded DNA. As a result, non-homologous strands of DNA can be joined, which “could lead to genomic instabilities—genome scars,” Hackl explained. This phenotype is also known as BRCAness.
BRCAness can contribute to high-grade serous ovarian cancer (HGSOC), which Hackl and his colleagues described as “the most lethal gynecologic malignancy despite new therapeutic concepts.” In an interview about this work, Hackl pointed out that “up to 50% of HGSOC patients could be associated with BRCAness.”
An HGSOC patient’s BRCAness impacts the response to treatment. As Hackl said, “BRCAness is of high relevance for therapy, since patients are more sensitive to platinum-based chemotherapy or poly-ADP-ribose polymerase—PARP—inhibitors.”
So Hackl and his colleagues performed immunogenomic analysis of several groups of HGSOC patients, and analyzed the results with machine-learning algorithms. Although there are FDA-approved methods of assessing BRCAness, usually based on next-generation sequencing of tumor DNA, Hackl noted that “machine-learning methods were very useful for classification of BRCAness based on gene expression—RNA sequencing—and particularly for feature-selection resulting in a prediction model including only 24 genes.”
In addition to these results, Hackl’s team created a web application—OvRSeq—and an R-based package. In combination, these can be used to analyze samples from patients with ovarian cancer. “The R package—although easy to use—is actually directed to researchers with a more bioinformatics-related background, whereas the web application is dedicated to more clinical-related researchers and oncologists to generate a report for each tumor sample,” Hackl explained.
To make use of these tools in the clinic, however, Hackl noted that “the challenges are more related to the clinical approval by authorities, such as the FDA.”
In the meantime, Hackl is working on applying his methods to combinations of immunotherapies. In ovarian cancer, for example, Hackl pointed out that only about 10% of patients respond to single immunotherapies. “It might be that a combination of checkpoint blockers and other inhibitors improve the outcome,” he said.
Improving cancer care in children
Immunogenomics might offer special promise for treating pediatric cancers—an area of great need. As reported by pediatric oncologist David Siegel, MD, of the Centers for Disease Control and Prevention’s division of cancer prevention and control, and his colleagues: “Cancer is a leading cause of death by disease among children and adolescents in the United States.”

pediatric oncologist
Sydney Children’s Hospital
Moreover, the impact of advanced therapies varies with pediatric cancers. “Some immunotherapies have worked very well in pediatric cancers, like CAR T cells for leukemia, but others—particularly checkpoint inhibitors—have really generally failed in most pediatric cancers,” said David Ziegler, MD, a pediatric oncologist at the Kids Cancer Centre, Sydney Children’s Hospital, in Australia. “We think that there is actually a role here, particularly around immunogenomics, to try and better select patients for these immunotherapies, because we know that there are outliers who do respond.”
Ziegler and his colleagues applied genomic analysis to children with high-risk cancers, meaning those with a cure rate that is probably 30% or less. In particular, this team looked at the impact of precision-guided treatments. This work included whole-genome sequencing, collecting data on the RNA transcriptome, and DNA-methylation profiling. From this work, Ziegler and his colleagues concluded that precision-guided treatments “informed by comprehensive molecular profiling significantly improves outcomes for children with high-risk cancers.”
In addition, Ziegler and his colleagues reviewed the use of immune profiling in search of what makes a child’s tumor more likely to respond to an immunotherapy, particularly checkpoint inhibitors. “From RNA analysis, we can pull out those tumors that we think will more likely respond to immune therapies and checkpoint inhibitors,” Ziegler says.
To perform such studies, Ziegler pointed out that “whole-genome sequencing, RNA sequencing, or DNA methylation profiling are sort of the easy parts, but doing the analysis really needs some sort of expertise and curation.” To optimize the data handling and analysis, “the team has developed profiling and curation tools that do a lot of that work automatically,” said Ziegler. “As soon as the RNA sequencing is done, one of the outputs that is automatically generated is a score—high or low—of how likely a tumor is to respond to immunotherapy.” By retrospectively applying this analysis to children who had received immunotherapy, said Ziegler says, they could identify the ones who actually responded to the treatment.

immunotherapies. [Hubert Hackl]
To further test this approach, Ziegler and his colleagues will soon start enrollment on a clinical trial. “It’s actually an arm of a basket trial where we will then be able to stream patients on to receive immunotherapy based on that transcriptomic profile,” he explained. “So, we’re hopeful that by selecting those patients based on that RNA sequencing, we may be able to find those who are going to respond.”
When cancer strikes the brain
Although all cancer is frightening for patients and their loved ones, special fear comes with brain cancer, and for good reasons. “Despite the use of aggressive multimodality therapies, the prognosis of brain tumor patients remains poor,” reported Andrea Pace, MD, a neurooncologist at the IRCCS Regina Elena Cancer Institute in Rome, and coauthors. In some brain cancers, the median survival age is measured in just months. Consequently, scientists around the world have been applying immunogenomics to brain cancer.
“Brain metastases (BrMs) are the most common form of brain tumors in adults and frequently originate from lung and breast primary cancers,” wrote Johanna Joyce, PhD, oncology professor at the University of Lausanne in Switzerland and president-elect of the European Association for Cancer Research. “BrMs are associated with high mortality, emphasizing the need for more effective therapies.” Current treatments for BrMs, according to these scientists, “are largely palliative.”
Joyce and her colleagues gathered blood samples and sections of metastatic brain tumors from surgeries from 21 patients whose cancer started in the lungs and 9 whose started in breast tissue. Then, the team used whole-exome and whole-genome sequencing, RNA sequencing of immune-system cells, analysis of tissue images, and more to characterize the immunogenomics of the BrMs.
The results showed distinct tumor immune microenvironments for lung and breast BrMs. These unique immunophenotypes of the tumor immune microenvironments, Joyce and her colleagues concluded, “can be of critical importance to predict responses to current immunotherapies, to stratify patients, and to develop novel immune-based personalized treatments guided by the genetic makeup of the tumors.”
Other scientists also apply immunogenomics to BrMs. Working with blood and brain tumor samples from 53 patients with cancers starting as breast cancer, melanoma, lung cancer, or renal cancer, Maria Ascierto, PhD, professor of translational cancer immunology at the Providence Saint John’s Health Center in Santa Monica, California, and her colleagues applied immunogenomic and spatial analysis. The gene expression and immune-cell profiles varied in these patients based on the source of the original cancer. For example, the melanoma-derived brain metastases were more immunogenic than non-melanoma-derived ones. Based on the results from this work, Ascierto and her colleagues proposed that “a balance between neuro-immune architectures might be associated with diverging clinical outcome of patients with BrMs.”
When it comes to brain cancers in children, considerable work remains for immunogenomics. As Natalie Jäger, PhD, a senior scientist at the German Cancer Research Center (DKFZ) in Heidelberg, and her colleagues reported: “While the tumour microenvironment in adults has been widely studied to delineate determinants of immune response, the immune composition of paediatric solid tumours remains relatively uncharacterized calling for investigations to identify potential immune biomarkers.”
To address this area, Jäger and her colleagues worked with RNA sequencing data from 925 nervous-system tumors in children who had yet to be treated. The data came from the Children’s Brain Tumor Network, the National Cancer Institute Therapeutically Applicable Research To Generate Effective Treatments initiative, and the International Cancer Genome Consortium. The tumors included 12 kinds of cancer, from choroid plexus tumors and neurofibroma to medulloblastoma and neuroblastoma.
Analysis of the transcriptional data across a dozen nervous-system tumors in children revealed four clusters of immune information that the scientists labeled as pediatric inflamed, myeloid predominant, immune neutral, and immune desert, which represent higher to lower levels of immune signals in the samples, respectively. Based on the immune variation between the tumors, Jäger and her colleagues suggested that “personalized immunogenomic profiling is needed to guide selection of immunotherapeutic strategies.”
Nervous-system cancers also go beyond the brain. As one example, Udai Kammula, MD, director of the solid tumor cell therapy program at the University of Pittsburg’s Hillman Cancer Center, and his colleagues studied uveal melanoma. The uvea comprises three parts of the eye: the iris, ciliary body, and the choroid. Kammula and his colleagues studied this rare version of melanoma because it resists immune checkpoint inhibitors. This research team used genomic, transcriptomic, and immune-cell data to analyze 100 unveal melanoma metastases. Despite this form of cancer being resistant to immunotherapies, Kammula’s team found tumor-infiltrating, but inactive lymphocytes in more than half of the samples. So the scientists developed a transcriptomic biomarker to identify tumor-infiltrating lymphocytes, and a method to extract and activate them. Lastly, Kammula’s team reported that “adoptive transfer of these transcriptomically selected tumor infiltrating lymphocytes can promote tumor immunity in patients with metastatic uveal melanoma when other immunotherapies are incapable.”
A collection of computational tools
Many scientists apply advanced computational methods when analyzing immunogenomic information. As one example, Xin Luan, PhD, a pharmacologist at the Shanghai University of Traditional Chinese Medicine in China, and his colleagues explored immunogenomic data in patients with lung adenocarcinoma (LUAD). These scientists gathered data from several sources—the Cancer Genome Atlas, the Genotype Tissue Expression project, and Gene Expression Omnibus database—and analyzed it with the LUAD Immunological Multi-Omics Classification system, which incorporates seven machine-learning algorithms. From this work, Luan and his colleagues identified three subtypes of LUAD and various genes associated with antigen-presenting cells, which could be targeted with mRNA-based vaccines.
As immunogenomics matures even further, increasingly sophisticated methods of computation will be required to optimize the value of the information. Nicola Waddell, PhD, head of the medical genomics group at the QIMR Berghofer Medical Research Institute in Brisbane, Australia, and her colleagues recently reviewed the use of computational immunogenomics as a tool for predicting the impact of cancer immunotherapies—especially the analysis of “bulk tissue and single-cell sequencing data from cancer, stromal and immune cells, as well as how best to select the most appropriate tool to address various clinical questions.” The answers to those questions could be used in developing a treatment plan for a patient.

“The establishment of large-scale genomic collaborative efforts along with the development of new single-cell transcriptomic techniques and multi-omics approaches have enabled characterization of the mutational and transcriptional profiles of many cancer types and helped to identify clinically actionable alterations as well as predictive and prognostic biomarkers,” Waddell and her colleagues wrote. “Researchers have developed computational approaches and machine learning algorithms to accurately obtain clinically useful information from genomic and transcriptomic sequencing data from bulk tissue or single cells and explore tumours and their microenvironment.”
In particular, Waddell and her colleagues pointed out the use of immunogenomic tools when considering treatments that include immune checkpoint inhibitors. As they noted, these treatments are “based on cancer-intrinsic and cancer-extrinsic features that can be identified with sequencing, including tumour mutational burden, neoantigens and the presence of immune cells.”
Computational approaches to immunogenomics, however, are not foolproof. As one example, Waddell and her colleagues mentioned that deconvolution tools—a computational approach that estimates the proportions of cell types in a sample—“have limitations in identifying low-abundance cell types and subsets” of immune cells in the tumor microenvironment. Consequently, the authors noted: “the use of these tools requires careful consideration of the underlying technical and biological factors.”
As in much of biology and medicine, computational immunogenomics applied to cancer benefits from bigger and better datasets. As Waddell and her colleagues put it: “Multi-omic machine learning models trained on molecular and clinical features from large cohorts of tumour samples could improve the prediction of patient responses to immunotherapy and reveal key predictive features.”
Immunogenomics is still information science
Today, getting close to a decade after Holt called immunogenomics an information science, the same might be truer than ever. The experts interviewed here along with a collection of studies on the application of immunogenomics to cancer show the centrality of data to advancing this field. Nonetheless, such advances depend on large amounts of high-quality data and tools to analyze it. In many cases, however high-quality data is lacking, especially data that is suitable for advanced analysis such as AI-based methods. Still, combining today’s best data with the most powerful analytical methods is showing scientists more about how various cancers progress, resist treatments, and how that resistance might be overcome.
Read more:
- Holt, R.A. Immunogenomics: a foundation for intelligent immune design. Genome Medicine 7: 116. (2015).
2. Gronauer, R., Madersbacher, L., Monfort-Lanzas, P., et al. Integrated immunogenomic analyses of high-grade serous ovarian cancer reveal vulnerability to combination immunotherapy. medRxiv. (2024).
3. OvRSeq. ovrseq.icbi.at
4. Siegel, D.A., King, J.B., Lupo, P.L., et al. Counts, incidence rates, and trends of pediatric cancer in the United States, 2003-2019. Journal of the National Cancer Institute 115(11):1337–1354. (2023).
5. Lau, L.M.S., Khuong-Quang, D-A., Mayoh, Ch. et al. Precision-guided treatment in high-risk pediatric cancers. Nature Medicine (online ahead of print). (2024).
6. Terry, R.L., Meyran, D., Ziegler, D.S., et al. Immune profiling of pediatric solid tumors. Journal of Clinical Investigation 130(7):3391–3402. (2020).
7. Pace, A., Tanzilli, A., Benincasa, D. Prognostication in brain tumors. Handbook of Clinical Neurology 190:149–161. (2022).
8. Álvarez-Prado, A.F., Maas, R.R., Soukup, K., et al. Immunogenomic analysis of human brain metastases reveals diverse immune landscapes across genetically distinct tumors. Cell Reports Medicine 4(1): 100900. (2023).
9. Mendoza-Valderrey, A., Dettmann, E., Hanes, D., et al. Immunogenomics and spatial proteomic mapping highlight distinct neuro-immune architectures in melanoma vs. non-melanoma-derived brain metastasis. BJC Reports 2: 38. (2024).
10. Nabbi, A., Beck, P., Delaidelli, A., et al. Transcriptional immunogenomic analysis reveals distinct immunological clusters in paediatric nervous system tumours. Genome Medicine 15: 67. (2023).
11. Leonard-Murali, S., Bhaskarla, C., Yadav, G.S., at al. Uveal melanoma immunogenomics predict immunotherapy resistance and susceptibility. Nature Communications 15: 2863. (2024).
12. Tian, S., Luo, M., Liao, X., et al. Integrated immunogenomic analysis of single-cell and bulk profiling reveals novel tumor antigens and subtype-specific therapeutic agents in lung adenocarcinoma. Computational and Structural Biotechnology Journal 23:1897–1911. (2024).
13. Addala, V., Newell, F., Pearson, J.V., et al. Computational immunogenomic approaches to predict response to cancer immunotherapies. Nature Reviews Clinical Oncology 21:28–46. (2024).
14. May, M. Massive attack: can biotechnology turn a bonanza of data into a boon? GEN Biotechnology 3(3):107–110. (2024).
Mike May is a freelance writer and editor with more than 30 years of experience. He earned an MS in biological engineering from the University of Connecticut and a PhD in neurobiology and behavior from Cornell University. He worked as an associate editor at American Scientist, and he is the author of more than 1,000 articles for clients that include GEN, Nature, Science, Scientific American, and many others. In addition, he served as the editorial director of many publications, including several Nature Outlooks and Scientific American Worldview.







![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




