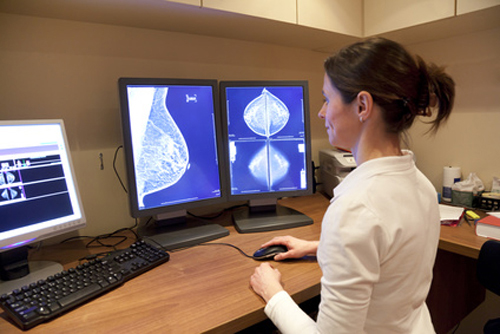
The world’s largest study on the use of AI-guided mammography screening to date has shown that the technology increases the rate of breast cancer detection without negatively impacting the recall rate.
The results, which are published in Nature Medicine, also highlight the potential of AI to reduce the workload of radiologists without compromising diagnostic quality.
The prospective PRAIM study included data for 463,094 women aged 50–69 years who underwent mammography screening at 12 sites in Germany between July 2021 and February 2023. All the women had their images reviewed independently by two radiologists, which is standard within Germany’s national breast cancer screening program, but in 56.3% of cases the review was assisted by AI.
“Our initial aim was to demonstrate that AI-based evaluations are equivalent to human assessments,” explained Prof. Alexander Katalinic, PhD, principal investigator and director of the Institute of Social Medicine and Epidemiology at the University of Luebeck and UKSH, Campus Luebeck. “However, the findings exceeded our expectations: AI significantly improves breast cancer detection rates.”
The AI system used in the study was Vara MG (from the German company Vara), which is a CE-certified medical device designed to display mammograms (viewer software) and preclassify screening examinations to assist radiologists in their reporting routine.
After image acquisition, AI predictions were computed for all women but were displayed only to radiologists who chose, on a per-examination basis, to use the AI-supported viewer. Examinations were assigned to the AI group when at least one of the two radiologists read and submitted the report with the AI-supported viewer.
When using the AI-supported viewer, the 119 radiologists who took part in the study were supported by two AI-based features:
- Normal triaging. The software selects a subset of all examinations deemed highly unsuspicious by the AI model. These examinations are tagged ‘normal’ in the worklist.
- Safety net. The software selects a subset of all examinations deemed highly suspicious by the AI model. Radiologists first read the screening examination without any further AI support. When the radiologists interpret an examination as unsuspicious, the safety net is activated with an alert and a suggested localization of the suspicious region in the images. The radiologists are then prompted to review their decision and either accept or reject the safety net’s suggestion.
After controlling for potential confounders, Katalinic and colleagues found that the breast cancer detection rate was 6.7 per 1000 women screened in the AI group and 5.7 per 1000 women screened in the control group. This represents one additional cancer case detected per 1000 screened women and a statistically significant relative increase of 17.6% with the use of AI.
Importantly, the researchers found that the number of women recalled for further assessment was similar between the two groups, at rates of 37.4 and 38.3 per 1000 in the AI and control groups, respectively.
Katalinic told Inside Precision Medicine that “increasing the sensitivity of screening procedures is very often associated with a decrease in specificity. This means that the number of false positive findings increases, which leads to relevant harm through additional examinations and anxiety among the screening participants.”
“The fact that the recall rate remains the same using AI is therefore a very important result of the study,” he said. “From the point of view of women without breast cancer, which is more than 99%, this is the decisive finding.”
Another key finding was the potential for AI to improve efficiency in breast cancer screening. Using simulated screening scenarios, the investigators showed that if none of the cases flagged as normal by AI were further reviewed by radiologists, the breast cancer detection rate would still be a significant 16.7% higher in the AI group. Furthermore, the number of unnecessary recalls was a significant 15.0% lower.
Katalinic also pointed out that “AI has shifted the reporting times of the double reading of the mammograms.” He said: “Cases that were tagged as normal by the AI were processed more quickly. Cases that were tagged as abnormal were viewed for longer (thus leading to an increase tumor detection). Although the setting of the study is that of a mass examination, AI can result in a more precise and targeted breast cancer detection.”
Given that radiologists in Germany currently analyze 24 million individual images annually, the implementation of AI could significantly alleviate their workload. “Based on our results, adding AI to human double reading makes sense and will improve mammography screening,” Katalinic remarked.
He added that the simulations the team carried out suggest that, in the context of double reading, it should be possible to replace at least one examiner with AI, although perhaps only in mammograms tagged as normal. “This should be discussed now to save the time of human physician for more meaningful tasks,” he said.
Stefan Bunk, chief technology officer of Vara, emphasized the global significance of the findings: “The PRAIM study highlights the immense potential of AI to enhance screening programs worldwide. This evidence will elevate discussions about integrating AI into healthcare systems to a new level.”
Future research will now focus on evaluating the long-term impact of AI on patient prognosis and its integration into routine clinical workflows.








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




