A new study has identified interleukin-6 (IL-6) as a promising diagnostic biomarker for the early detection of sepsis in high-risk patients, including newborns, children, and pregnant women. Results were presented at the European Society of Clinical Microbiology and Infectious Disease (ESCMID) Global 2025 in Vienna, Austria.
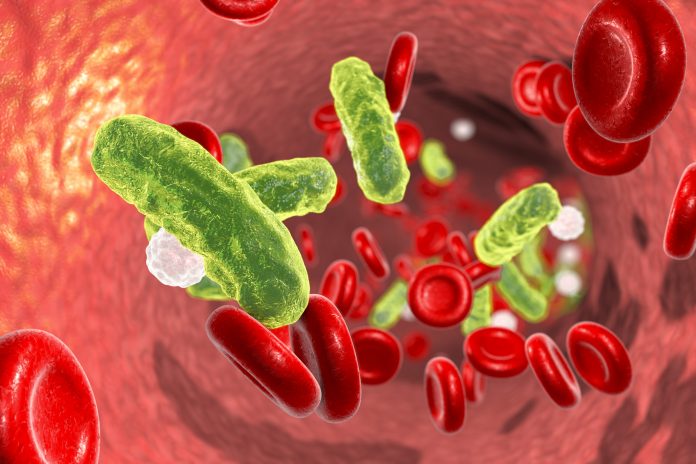
Sepsis is one of the most frequent causes of death worldwide, with almost half of all cases affecting children under five years of age. In addition to newborns and young children, pregnant women are highly vulnerable to contracting sepsis due to the immunological changes caused by pregnancy. This study is the first to evaluate the diagnostic performance of IL-6 in a real-world cohort across these three patient populations.
Early sepsis detection is critical to improve patient outcomes, as the condition progresses rapidly. However, the nonspecific symptoms of sepsis, which can be caused by a wide range of pathogens, make diagnosis challenging. Traditional diagnostic biomarkers of sepsis, including C-reactive protein (CRP) and procalcitonin (PCT), show a delayed response and low sensitivity, hindering early detection. In comparison, IL-6 can offer a much earlier detection window.
“IL-6 secretion rises within 1–2 hours, peaks at 6 hours, and decreases by 24 hours, whereas CRP and PCT peak much later at 48 and 24 hours, respectively,” said Seán O. Whelan, PhD, first author of the study and clinical microbiologist at Children’s Health Ireland at Temple Street. “This faster, steeper response makes IL-6 a promising biomarker for earlier sepsis detection.”
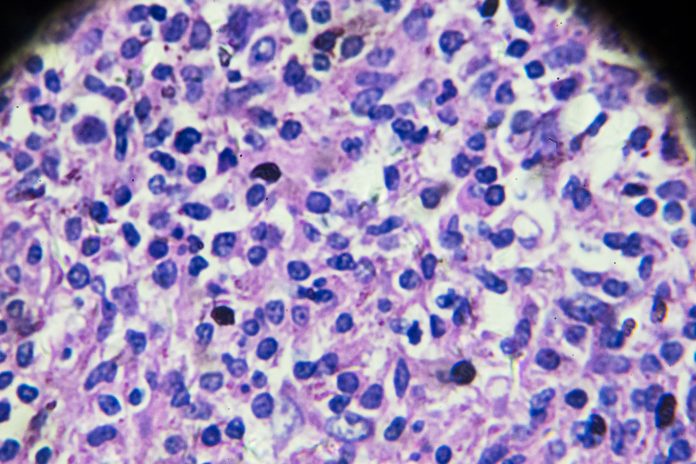
The diagnostic accuracy of IL-6 was analyzed in a retrospective cohort study that enrolled a total of 252 patients with suspected sepsis, including 111 pediatric, 72 maternity, and 69 neonatal cases. Results showed that IL-6 outperformed CRP and PCT in distinguishing bacterial and non-bacterial infections, with an area under the receiver operating characteristic (AUROC) value of 0.94 in maternity patients, 0.91 in children, and 0.86 in newborns. Participants were also stratified according to sepsis severity, with IL-6 effectively distinguishing between mild infection, sepsis, and septic shock stages.
While IL-6 showed high sensitivity in children (91%) and pregnant women (94%), sensitivity was lower in the neonate group. The researchers attributed this, in part, to the complex diagnosis of neonatal sepsis and the lack of a clear consensus definition of diagnostic criteria.
“Our findings reinforce the potential of IL-6 as a promising biomarker in sepsis diagnosis,” said Whelan. “IL-6 is already in routine use in our institutions, the Rotunda Hospital and Children’s Health Ireland at Temple Street, for these populations. With wider adoption and in combination with clinical assessment, IL-6 could significantly improve clinical decision-making and support timely, targeted treatment for high-risk patients.”








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




