The immunotherapy afamitresgene autoleucel (afami-cel) for the treatment of adults with the rare soft tissue cancer called synovial sarcoma was granted accelerated approval late last week by the U.S. Food and Drug Administration (FDA). Afami-cel is the first engineered T cell therapy to receive FDA approval for treatment of a solid tumor.
“This treatment offers an important new option for people with this rare cancer,” said Sandra D’Angelo, MD, a sarcoma specialist who led the clinical at Memorial Sloan Kettering Cancer Center (MSK). “It is also an important step forward in the development of T cell therapies for solid tumors, which has been a major challenge.”
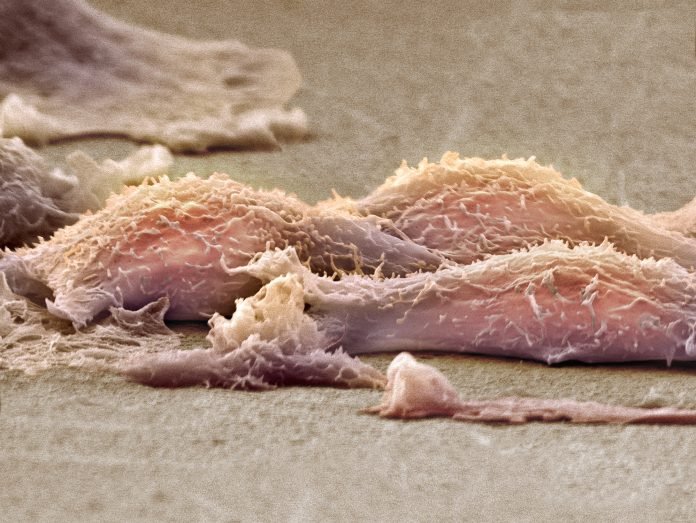
Chimeric antigen receptor (CAR) T cell therapies have been effectively treating various forms of blood cancer since 2017 and work by targeting proteins on the surface of cancer cells. But development of CAR T therapies for treating solid tumors have encountered numerous roadblocks to being effective including off-target effects due to lack of specific target antigens, T cell exhaustion, and tumor heterogeneity, among others.
Afami-cel is not a CAR T therapy, rather it is a T cell receptor (TCR) therapy. Related to CAR Ts, TCRs can target proteins within the cell itself, while CAR T therapies only target proteins on the cell surface. The cell engineering process for afami-cel, however, is virtually the same as for CAR T cell therapies: a patient’s T cells are collected from their blood, then engineered to recognize and fight a specific target in cancer cells, which are then reinfused into the patient.
The target for afami-cel is a a protein called MAGE-A4.
The FDA approval for afami-cel was based on results from Adaptimmune’s pivotal SPEARHEAD-1 trial for treating metastatic synovial sarcoma and myxoid round cell liposarcoma (MRCLS), results of which were published in April in The Lancet. MRCLS is a distinct disease that shares clinical and biological features with synovial sarcoma including the expression of the MAGE-A4 cancer antigen.
In total, 52 patients were treated with afami-cel (44 with synovial sarcoma, eight with myxoid round cell liposarcoma). All patients had not responded to earlier lines of therapy. Data from the trial showed that 37% of the patients had their tumors shrink after receiving a single dose. Efficacy rates were 39% for synovial sarcoma patients and 25% in those with MRCLS.
Synovial sarcoma patients responded to their treatment for an average of 11.6 months; MRCLS patients for an average of 4.2 months. D’Angelo, who was the lead author the The Lancet piece noted that these responses were important for this group of patients as many had exhausted all other treatment options.
Prior to receiving the therapy, all patients enrolled in the trial received chemotherapy. Hematologic toxicities were the most common adverse events, which the investigators expected as a result of lymphodepletion which commonly occurs in chemotherapy patients. Cytokine release syndrome (CRS), a potentially serious side effect, was experienced by 71% of trial participants, though symptoms of CRS were not severe for most patients.
With this first approval in hand, the hope is afami-cel can be approved in the future for other indications in which the tumor carries the mutated MAGE-A4 protein. The immunotherapy is now also being studied in pediatric sarcomas.





