
Extended estrogen suppression in postmenopausal breast cancer does not increase patients’ risk of coronary artery calcification, as some prior studies had indicated, new evidence from an international collaboration shows. This finding helps address a key issue in treating this population
Aromatase inhibitors are a mainstay in treating hormone receptor-positive postmenopausal breast cancer. Meanwhile, coronary artery calcification is a significant predictor of heart disease. Balancing the benefits of estrogen suppression with the risk of heart disease has been a key issue in this field.
This study appeared in the Canadian Journal of Cardiology and the lead investigator is Yu Hiasa, MD, department of cardiology, pulmonology, hypertension & nephrology, Ehime University Graduate School of Medicine, Japan. The study is a retrospective, cross-sectional observational analysis that investigated the association between the duration of aromatase inhibitor treatment and the severity of coronary artery calcification in postoperative breast cancer patients.
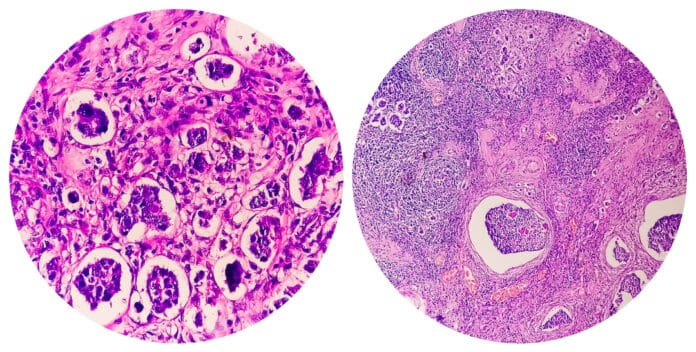
Coronary artery calcification is believed to be associated with atherosclerosis, which causes angina and heart attacks. Estrogen has a beneficial role in cardiovascular health, but its suppression is often necessary in breast cancer treatment. Hormonal therapy, particularly the use of aromatase inhibitors (which block the production of estrogen), is a standard treatment after breast cancer surgery for postmenopausal women. These therapies are effective in reducing cancer recurrence, but there has been increasing concern about their potential cardiovascular side effects, including acceleration of coronary artery atherosclerosis.
Hiasa said, “Although there is an ongoing discussion on the optimal duration of aromatase inhibitor therapy (5 years or 10 years), our data suggest that longer aromatase inhibitor use (as often used to prevent or suppress late recurrences or spread of breast cancer) is safe, at least in regard to coronary artery calcification.”
The study included 357 postmenopausal breast cancer patients who initiated adjuvant endocrine therapy with aromatase inhibitors for breast cancer. Coronary artery calcification was quantified using a visual ordinal scoring system, and patient characteristics were assessed based on the presence of coronary artery calcification. Independent risk factors for elevated coronary artery calcification scores were identified through a multivariable logistic regression model.
Co-investigator Akinori Higaki, MD, PhD, also of Ehime University Graduate School of Medicine, said “Our analysis of the postoperative breast cancer patient cohort revealed that the duration of treatment with aromatase inhibitors and the presence of osteoporosis were not associated with coronary artery calcification.“
In addition to the well-known risk factors for coronary artery calcification such as older age, hypertension, and diabetes mellitus, researchers found that a lower hemoglobin level is also an independent risk factor for coronary artery calcification.
In an accompanying editorial, Ibrahim Alfaris, division of cardiovascular medicine, Stanford University School of Medicine, wrote, “Identifying low hemoglobin as a novel, highly significant risk factor for coronary artery calcification in this population raises the possibility of adding anemia as an indication for cardiovascular screening. Anemia is not typically noted in classic atherosclerotic cardiovascular disease risk calculators or expert recommendations, and this finding could lead to changes in screening practices for postmenopausal women undergoing aromatase inhibitors therapy.”









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




