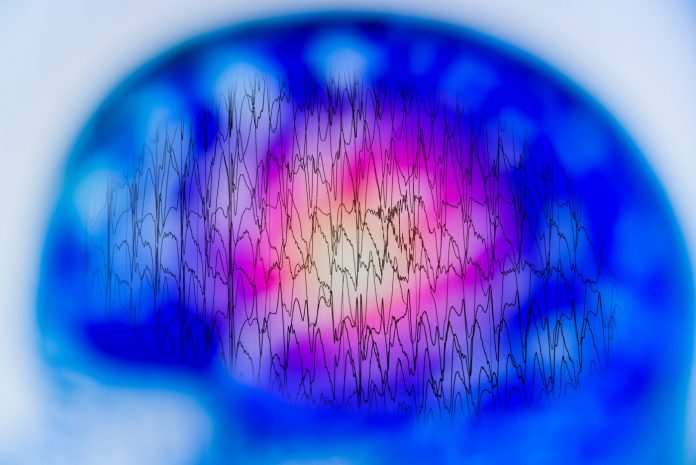
The story so far: In late November, news of the success of a drug to reduce cognitive decline in patients with Alzheimer’s disease burst on the horizon with all the promise of being a silver bullet. The drug, lecanemab, jointly developed by pharma companies Biogen and Eisai, was tested on patients with early Alzheimer’s. Results of the study presented at the Clinical Trials on Alzheimer’s Disease conference in San Francisco, U.S., and published in the New England Journal of Medicine (NEJM) showed modest effects in arresting decline in cognitive and functional aspects in patients with early disease. This has sparked hope in a world where an estimated 55 million people live with the debilitating effects of Alzheimer’s disease.
What is lecanemab and how does it work?
Lecanemab belongs to a class of drugs called monoclonal antibodies. These antibody-mediated drugs target beta amyloid, the protein deposition that is seen in patients with Alzheimer’s disease, and disrupts cells function.
Neuropsychiatrist Ennapadam. S. Krishnamoorthy, founder, Buddhi Clinic, Chennai, says: “For years amyloid plaques have thought to be an important target for treatment in Alzheimer’s. This class of drugs does precisely that.”
As per the NEJM paper, the clinical trial, conducted over 18-months, a multi-centre, double-blind, phase 3 trial, involved persons 50 to 90 years of age with early Alzheimer’s disease (mild cognitive impairment or mild dementia due to Alzheimer’s disease) with evidence of amyloid deposition. Participants were randomly assigned intravenous lecanemab or placebo. It was observed that lecanemab “robustly removed the amyloid plaques.”
This was the primary end point of the trial, which showed a change in the score recorded at baseline when the trial began on the Clinical Dementia Rating–Sum of Boxes (CDR-SB). Key secondary end points included a change in amyloid burden on PET (positron-emission topography). There were changes both in the lecanemab group versus the placebo group, the researchers concluded.
Will lecanemab be the silver bullet to treat Alzheimer’s?
The Lancet, in an editorial, argues that a phase-3 trial showing efficacy on clinical outcomes, particularly after such a long and fruitless wait for a successful therapy for Alzheimer’s disease, is welcome news.
However, it points out that the difference noticed on the CDR-SB scale may not be clinically meaningful, going by metrics indicated in previous studies. Also, the development of amyloid-related imaging abnormalities (ARIA) in one of five patients was a cause for concern.
The Lancet editorial concludes that given these concerns, “whether lecanemab is the game changer that some have suggested remains to be seen.” It goes on to explain that ongoing trials are assessing the efficacy of subcutaneous administration and whether lecanemab can prevent onset of dementia in patients with amyloid pathology but no clinical symptoms. “However, the immediate impact of lecanemab should not be overstated.”
Dr. Krishnamoorthy said the first of the drugs for Alzheimer’s — aducanumab — was approved in fast-track mode, to much criticism. “Many experts were unhappy with the trial results that led to its approval. Apart from the questionably small differences between the trial and placebo groups, a concern was expressed also about serious side effects like haemorrhages in the brain and oedema (brain swelling).”
Lecanemab, he adds, on the other hand, appears to have shown modest effects in early dementia both via clinical improvements (scores in the CDR and ADAS-Cog rating scales) and reduction in amyloid plaques. “The same problems of brain swelling and haemorrhages may exist with this drug as well, and may be true for many antibody-mediated treatments,” he explains.
For practitioners like him, this is an opportunity to be ‘cautiously optimistic’. “This is definitely a step forward and offers hope with the following caveats, including eligibility criteria, intensity of treatment, need for imaging and high costs.” Only those in the early course of the disease are likely to benefit. It has to be delivered via weekly IV injections requiring hospital visits and close monitoring, and in order to identify amyloid deposits, an amyloid PET, which is not available in many countries in the developing world, is required. The cost, as The Lancet speculates, is likely to be prohibitive for low-income and middle-income countries where most people with dementia live.
What is the future?
An initial decision on the drug’s approval by the FDA is expected by January 6, 2023, and from the European Medicines Agency later in 2023, according to The Lancet. The results on lecanemab, it argues, “might well pave the way for much needed treatments for Alzheimer’s disease. But for now, the key public health message for Alzheimer’s disease remains that laid out in the 2020 Lancet Commission on dementia prevention, intervention, and care: target the modifiable risk factors for dementia—such as hypertension, smoking, diabetes, and obesity—to maintain brain health across the lifespan”.






![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




