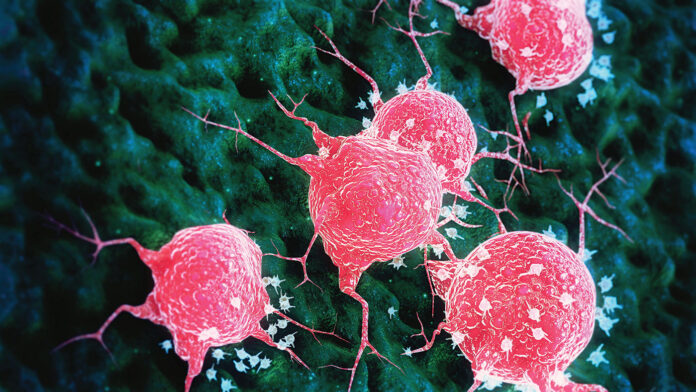
Small extracellular vesicles (sEVs) have emerged as powerful tools in cancer research. sEVs have been used as biomarkers for tumor diagnosis and as drug delivery vehicles. Researchers at the Perelman School of Medicine at the University of Pennsylvania have now refined these tools by engineering sEVs made from natural killer (NK) cells to target death receptor 5 (DR5), a protein that induces apoptosis in cancer cells. Their experimental approach suppressed tumor growth and improved survival in models of melanoma, breast, and liver cancers, which paves the way for new immunotherapies for solid tumors.
The findings are published in Science Advances and led by Xiaowei “George” Xu, MD, PhD, professor of pathology and laboratory medicine, and member of the Tara Miller Melanoma Center in Penn Medicine’s Abramson Cancer Center.
CAR-T cell therapies have been a game changer in the treatment of blood cancers. However, CAR-T cell application in solid tumors remains challenging. There is an unmet clinical need for better cellular therapies for solid tumors. The team of researchers sought to overcome this challenge.
DR5 is a protein on the surface of some cancer cells that can be activated to induce apoptosis, or cell death. Researchers have been trying for more than 20 years to develop successful DR5-targeting cancer treatments.
For their approach, the team used sEVs made by NK cells. Xu and his team engineered the NK sEVs so that they have an antibody fragment that strongly binds to and activates DR5. In lab-dish experiments, the sEVs specifically move toward and bind to DR5 and kill cancer cell types that have high levels of DR5 expression, including melanoma, liver, and ovarian cancer cells. In experiments with mouse models of melanoma, breast, and liver cancers, the sEVs strongly suppressed tumor growth and prolonged survival.
“Here, we engineered NK92 cells to secrete sEVs with DR5 agonistic [single-chain variable fragment] scFvs on the surface,” the researchers wrote. “Platelet-derived growth factor receptor (PDGFR) transmembrane domain (TM) delivers more DR5-scFvs to the surface of sEVs than CD8 TM. Live cell imaging studies showed that DR5-scFv sEVs rapidly induced apoptosis of DR5+ melanoma cells. The engineered sEVs specifically migrated to DR5+ melanoma cells in vitro and in vivo. Systemic delivery of DR5-scFv sEVs significantly inhibited the growth of multiple cancer types and prolonged the life span of treated mice. Adverse reactions in the treated mice were not observed.”
Not only did the tiny anticancer weapon pack a powerful punch, but multiple punches: the sEVs attacked other DR5-expressing cells called cancer-associated fibroblasts and myeloid-derived suppressor cells, which tumors use to create an immune-suppressive environment around themselves. The sEVs also stimulated T cells, giving another boost to anticancer immune activation.
“Furthermore, DR5-scFv sEVs significantly inhibited MDSCs and cancer-associated fibroblasts (CAFs) in the TME and activated CD8+ T cells in organotypic patient-derived melanoma slice culture models,” noted the researchers. “Together, DR5-scFv sEVs inhibit tumor growth by targeting tumor cells and immunosuppressive stromal cells in the TME.”
Xu noted that sEVs can be manufactured and stored relatively easily, making them a potential “off-the-shelf” therapy that could be given to any patient and would not require retrieving cells from each patient, as is the case with other personalized cellular therapies.
The team plans to refine the manufacturing process to scale production for clinical-grade sEVs and conduct safety studies to prepare for human clinical trials.





