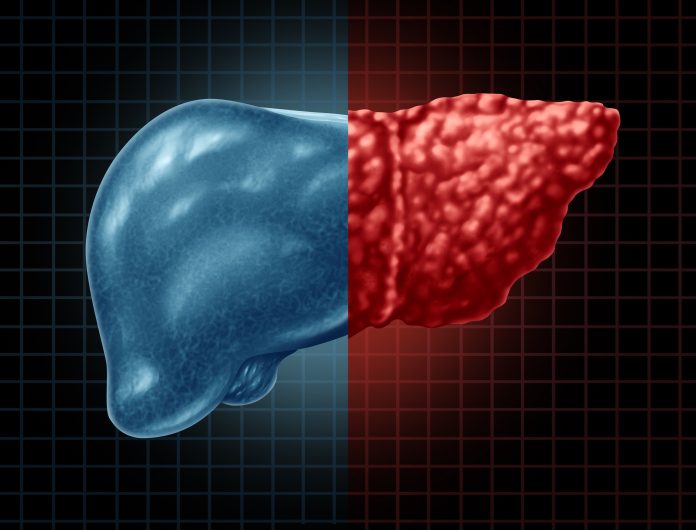
A new study has identified two distinct subtypes of metabolic dysfunction-associated steatotic liver disease (MASLD)—formerly known as nonalcoholic fatty liver disease (NAFLD)—a fatty liver disease that can progress to cirrhosis, liver cancer, and other health complications. The disease spans from benign fat accumulation in the liver (steatosis) to its more severe form, metabolic dysfunction-associated steatohepatitis (MASH, formerly nonalcoholic steatohepatitis or NASH). The research, led by Profs. François Pattou, MD, and Stefano Romeo, PhD, at Lille University Hospital, France, and published in Nature Medicine, will help clinicians better identify methods to tailor treatment for patients with this highly heterogenous disease.
The researchers included collaborators in Sweden, Italy, Belgium, and Finland. They named the two subtypes Liver-Specific MASH and Cardiometabolic MASH by using data based on histology and imagining from a number of European cohorts and the UK Biobank.
Liver-Specific MASH is genetically driven subtype characterized by a rapid progression of liver disease but low risk of cardiovascular effects. Cardiometabolic MASH is a high-risk form of the disease linked to type 2 diabetes and cardiovascular disease, similar to liver disease progression.
The researchers noted that this discovery is groundbreaking since both subtypes show very similar histological features both when examined with a microscope and on imaging—making them indistinguishable using traditional diagnostic methods. The team said that clinical approaches to treatment can now leverage readily available markers of the disease including age, body-mass index (BMI), HbA1c, LDL, cholesterol, triglycerides, and ALT to stratify MASH patients to personalized treatment approaches.
“This manuscript offers a transformative perspective on MASH and its heterogeneous outcomes,” noted an anonymous reviewer of the research. “Thoughtfully conducted on large, well-characterized cohorts, it opens new doors for precision medicine in this field.”
Distinct profiles and risks
Liver-Specific MASH is often associated with specific genetic variants, such as the minor allele of PNPLA3 rs738409, and has a stronger genetic predisposition for hepatic fat accumulation. In contrast, Cardiometabolic MASH is characterized by dyslipidemia, hypertension, and dysglycemia, suggesting a more systemic metabolic dysfunction.
“The two newly defined types of MASLD could be robustly identified in several independent and well-characterized cohorts, using a simple algorithm based on six widely available traits: age, BMI, HbA1c, ALT, LDL cholesterol and triglycerides,” the researchers wrote. The team also discovered that Cardiometabolic MASH was linked to unique lipid metabolism disturbances and alterations in immune response pathways, while Liver-Specific MASH was primarily driven by genetic factors affecting liver fat storage and transport.
Both subtypes showed elevated liver enzyme levels and increased risk for chronic liver disease, but only Cardiometabolic MASH was strongly associated with cardiovascular disease and diabetes.
Identifying the two distinct subtypes of MASH “sheds light on why current treatments often yield inconsistent results,” the researchers further noted. The research suggests that therapies like the thyroid hormone receptor agonist Resmetirom—which reduces liver fat content and inflammation—could be an effective treatment for Liver-Specific MASH; while Cardiometabolic MASH may respond better to drugs that regulate lipid and glucose metabolism, such as pegozafermin (a fibroblast growth factor 21 analog) or the GLP-1 receptor agonist semaglutide which also address cardiovascular risks.
“The newly proposed stratification could help refine emerging therapeutic strategies based on specific molecular pathomechanisms underlying each MASLD endotype,” the researchers noted.
The researchers acknowledged that further studies are needed to validate the findings in diverse populations and explore how these subtypes respond to different treatments. “We’ve always known MASH was heterogeneous,” Romeo concluded. “Now, we finally have a roadmap to turn these insights into real-world solutions for patients.”









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




