Researchers from Brigham and Women’s Hospital studied the link between sugar-sweetened beverages and the risk of liver cancer and chronic liver disease mortality. The study found that postmenopausal women consuming daily sugar-sweetened drinks had a significantly higher risk of these liver-related outcomes compared to those consuming fewer drinks.
Around 65% of U.S. adults drink sugar-sweetened beverages on a daily basis.
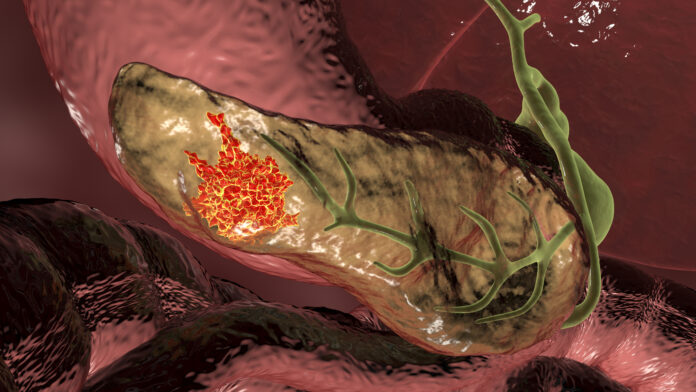
Around 65% of American adults regularly consume beverages sweetened with sugar. Chronic liver disease stands as a predominant source of illness and death globally, potentially leading to liver cancer and fatalities associated with liver diseases.
Researchers from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, led one of the first studies to look at the association between intake of sugar-sweetened beverages, artificially sweetened beverages, and the incidence of liver cancer and chronic liver disease mortality. The results of the study were recently published in the journal JAMA.
“To our knowledge, this is the first study to report an association between sugar-sweetened beverage intake and chronic liver disease mortality,” said first author Longgang Zhao, Ph.D., of the Brigham’s Channing Division of Network Medicine. Zhao is a postdoctoral researcher who works with senior author Xuehong Zhang, MBBS, ScD, in the Channing Division. “Our findings, if confirmed, may pave the way to a public health strategy to reduce the risk of liver disease based on data from a large and geographically diverse cohort.”
This observational study included nearly 100,000 postmenopausal women from the large, prospective Women’s Health Initiative study. Participants reported their usual soft drink, and fruit drink (not including fruit juice) consumption, and then reported artificially sweetened beverage consumption after three years. Participants were followed for a median of more than 20 years. Researchers looked at self-reported liver cancer incidence and death due to chronic liver disease such as fibrosis, cirrhosis, or chronic hepatitis, which were further verified by medical records or the National Death Index.
A total of 98,786 postmenopausal women were included in the final analyses. The 6.8 percent of women who consumed one or more sugar-sweetened beverages daily had an 85 percent higher risk of liver cancer and 68 percent higher risk of chronic liver disease mortality compared to those who had fewer than three sugar-sweetened beverages per month.
The authors note that the study was observational, and causality cannot be inferred and relied on self-reported responses about intake, sugar content, and outcomes. More studies are needed to validate this risk association and determine why sugary drinks appear to increase the risk of liver cancer and disease. Furthermore, more research is needed to elucidate the potential mechanisms by integrating genetics, preclinical and experimental studies, and -omics data.
Reference: “Sugar-Sweetened and Artificially Sweetened Beverages and Risk of Liver Cancer and Chronic Liver Disease Mortality” by Longgang Zhao, Xinyuan Zhang, Mace Coday, David O. Garcia, Xinyi Li, Yasmin Mossavar-Rahmani, Michelle J. Naughton, Melissa Lopez-Pentecost, Nazmus Saquib, Aladdin H. Shadyab, Michael S. Simon, Linda G. Snetselaar, Fred K. Tabung, Deirdre K. Tobias, Trang VoPham, Katherine A. McGlynn, Howard D. Sesso, Edward Giovannucci, JoAnn E. Manson, Frank B. Hu, Lesley F. Tinker and Xuehong Zhang, JAMA.
DOI: 10.1001/jama.2023.12618
Naughton reported grants from the National Institute of Aging (NIA) to The Ohio State University (to support the analysis and use of the Women’s Health Initiative [WHI] data for multiple publications during the conduct of the study; and grants from Merck Foundation (to support a research project not related to this article) outside the submitted work. Tobias reported grants from the National Cancer Institute (NCI) and grants from the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK) during the conduct of the study. VoPham reported personal fees from Georgetown University (speaker honorarium); and grants from NIH/NIDDK (K01 DK125612), NIH/NCI (P20 CA252732; P30 CA015704), and NIH/NHLBI (National Heart, Lung, and Blood Institute; 75N92019R0030) outside the submitted work. Dr Manson reported grants from NIH during the conduct of the study and grants from NIH and Mars Edge outside the submitted work. No other disclosures were reported
The Women’s Health Initiative program is funded by the US Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C. Zhang is supported by NIH/NCI grants (R21 CA238651, R21 CA252962, R37 CA262299, U01 CA259208, and U01 CA272452), an American Cancer Society Research Scholar Grant (RSG-17-190-01-NEC), and an American Cancer Society Interdisciplinary Team Award (PASD-22-1003396-01-PASD).