Researchers from the Johns Hopkins Kimmel Cancer Center and the Johns Hopkins University School of Medicine have developed a computational method to assess which patients with metastatic triple-negative breast cancer could benefit from immunotherapy. The work, published in the Proceedings of the National Academy of Sciences, aims to develop a more accurate measure for the stratification of responders and non-responders to this form of cancer treatment.
“It’s really important that we identify those patients for whom (immunotherapy) will work, because the toxicity of these treatments is high,” said lead study author Theinmozhi Arulraj, PhD, a postdoctoral fellow at Johns Hopkins.
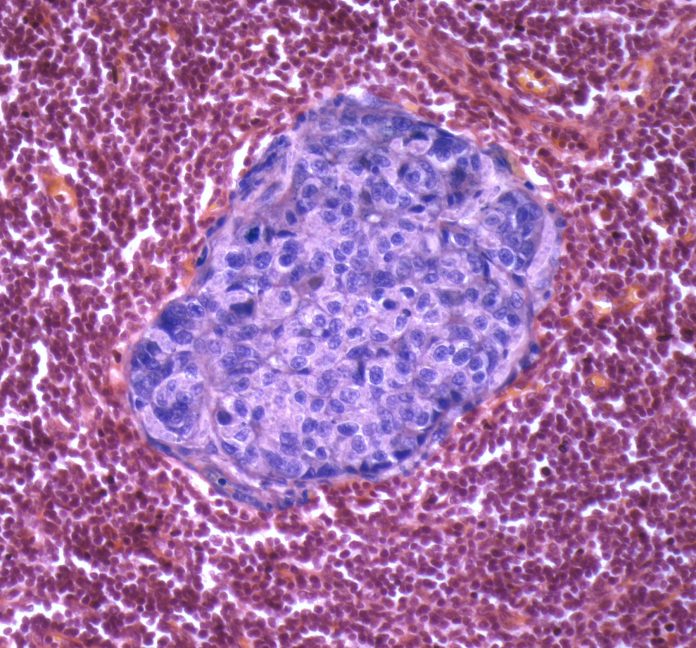
Previous research has focused on the presence or absence of specific cells and the expression of various molecules within tumors as biomarkers to delineate responders from non-responders, to allow clinicians to provide the right treatment to the right patients.
“Unfortunately, existing predictive biomarkers have limited accuracy in identifying patients who will benefit from immunotherapy,” said senior study author Aleksander Popel, PhD, a professor of biomedical engineering and oncology at Johns Hopkins. “Moreover, a large-scale assessment of characteristics that predict treatment response would require the collection of tumor biopsies and blood samples from many patients and would involve performing several assays, which is very challenging.”
To overcome this challenge, the Johns Hopkins team employed a quantitative systems pharmacology mathematical model to simulate profiles of more than 1,600 patients with metastatic triple-negative breast cancer and then simulated treatment with the approved immunotherapy pembrolizumab. This virtual clinical trial employed statistical and machine-learning approaches that sought to digitally identify biomarkers to indicate the potential for response, or non-response, to the drug in the simulated patient cohort.
Leveraging the synthetic data created by this computational exercise, the team then examined the performance of 90 biomarkers—both independently and in combinations. Their findings showed that tissue biopsies or blood biopsies taken before the start of therapy to search for pre-treatment biomarkers had limited the ability to predict treatment outcomes. However, they also showed that similar analysis of patients after the start of treatment querying on-treatment biomarkers, were better predictive markers of response and patient prognosis. Interestingly, the researchers also found that some commonly used biomarkers, such as PD-L1 expression and the presence of lymphocytes in the tumor performed better before the start of treatment rather than after treatment began.
Additionally, the team explored the potential of less invasive methods for predicting treatment responses and found that immune cell counts in the blood yielded comparable results to more invasive biopsy measures, suggesting a possible avenue for less intrusive patient testing.
Finally, the investigators sought to determine the predictive ability of tumor diameter, leveraging imaging from CT scans. “This, measured very early within two weeks of treatment initiation, had a great potential to identify who would respond if the treatment were continued,” Popel noted.
To validate these initial findings, the researchers conducted a virtual trial focused on patients whose tumor diameter changed within two weeks of starting treatment. Arulraj noted that the simulated response rates increased more than two-fold, from 11–25%, a “remarkable” increase.
“This emphasizes the potential for noninvasive biomarkers as an alternative, in cases where collecting tumor biopsy samples is not feasible,” he said.
Study co-author Cesar Santa-Maria, MD, an associate professor of oncology and breast medical oncologist at the Johns Hopkins Kimmel Cancer Center, said that combining both non-invasive markers of response with predictive models is key to helping clinicians tailor treatment plans.
“The complexities of the tumor microenvironment make biomarker discovery in the clinic challenging, but technologies leveraging insilico modeling have the potential to capture such complexities and aid in patient selection for therapy,” he said.





