Early-stage research led by the University of Rochester has uncovered a protein that is overproduced in the eyes of people with the eye disease age-related macular degeneration (AMD) and three similar disorders.
According to the Developmental Cell article, the protein, tissue inhibitor of metalloproteinases 3 (TIMP3), is produced in overly large quantities in people with AMD and similar conditions and this leads to inhibition of enzymes in the eye called matrix metalloproteinases.
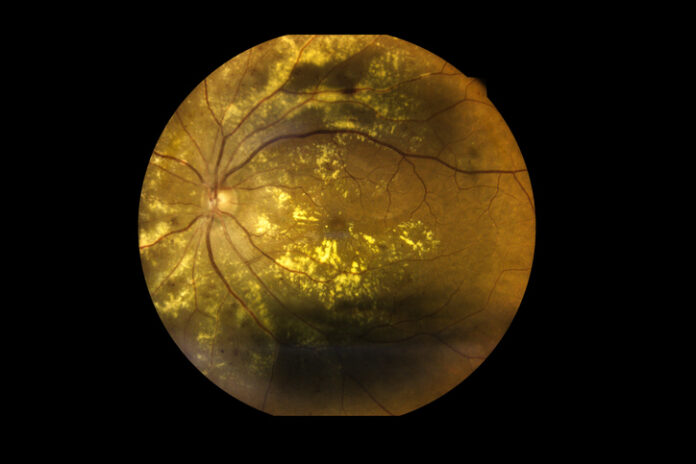
These enzymes are important for eye health and the research showed if they are inhibited this results in inflammation and the formation of drusen, plaque-like buildup of lipids and proteins in the retina, which are seen in the eyes of people with dry AMD and similar types of macular degeneration.
Notably, the researchers used a small molecule to block the inflammation caused by low matrix metalloproteinase levels and this appeared to reduce the formation of drusen in the lab-based model.
Around 20 million Americans over the age of 40 years have AMD and it is a leading cause of blindness in the U.S. There are two main forms, wet and dry AMD. Wet AMD involves the formation of abnormal blood vessels under the macular that cause blood and other fluids to leak into the retina. In contrast, dry AMD involves the formation of drusen in the macula that are gradually formed from cellular debris.
“Current treatments for AMD have limited efficacy and often come with significant side effects,” said lead author Ruchira Singh, PhD, a researcher at the University of Rochester Flaum Eye Institute and Center for Visual Sciences, in a press statement. “Our research aims to identify novel therapeutic targets that could potentially halt the progression of this disease.”
Singh and colleagues used human induced pluripotent stem cell (iPSC)-derived retinal pigment epithelium from patients with AMD and three distinct macular dystrophies—Sorsby’s fundus dystrophy, Doyne honeycomb macular dystrophy, and autosomal dominant radial drusen—to create a lab-based model for their study.
They found that in drusen forming macular degeneration, reduced activity of matrix metalloproteinase 2 leads to increased levels of the pro-inflammatory enzyme secretory phospholipase 2-IIA and drusen formation. Targeting this inflammatory enzyme with a small molecule inhibitor combined with supplementation with the kind of matrix metalloproteinase 2 found in the retina reduced drusen formation in the cell models of the different types of macular degeneration.
“Cellular pathways involved in drusen formation are key drivers of AMD progression,” said Singh. “If we can halt the accumulation of drusen, we may be able to prevent the disease from progressing to a stage where vision loss occurs. This research offers hope for developing new treatments that could significantly improve the lives of millions of people affected by AMD.”





