New discoveries made by researchers from the University of California, San Francisco (UCSF) introduce a sophisticated method to program CAR T cells, equipping them with a “zip code” system that enhances their precision in targeting brain tumors while minimizing collateral damage to healthy tissue. This innovative approach, which incorporates two-factor authentication-like mechanisms, holds promise for treating not only glioblastoma but also other central nervous system (CNS) disorders, such as neuroinflammation and metastases from other cancers. The new technique is published in a paper in Science.
Engineering the “zip code” approach
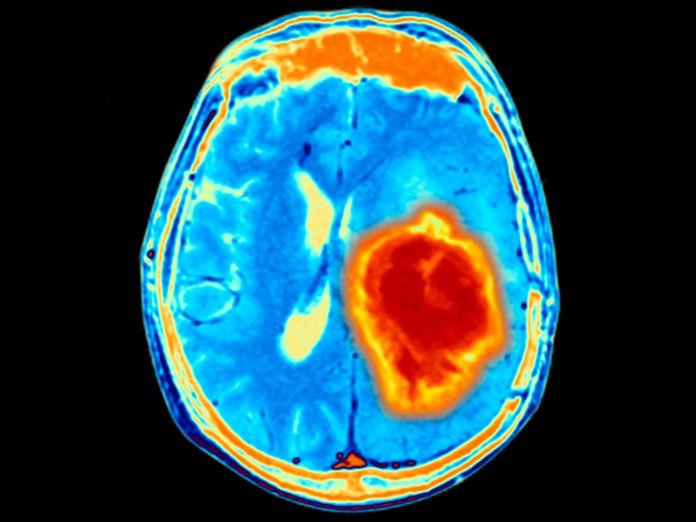
The brain has long posed unique challenges for therapy due to the need to navigate the blood-brain barrier while avoiding unintended effects on normal tissues. The UCSF team’s solution is to program T cells to recognize specific molecular markers within the brain’s extracellular matrix, the structural framework unique to this organ.
Traditional therapies often target a single molecular marker, akin to mailing a letter with only a street address. This can result in off-target effects, as the same molecular marker may exist in other tissues. The team developed a more nuanced strategy: “It’s better to mail a letter with a zip code and a street address,” explained co-senior author Wendell Lim. “With a living cell, this is what they typically do. They have instructions about where to go in the body, and then they look for molecular targets.”
To achieve this, the team leveraged brevican, a protein abundantly found in the brain’s extracellular matrix. “We engineered synNotch receptors that can recognize [brevican] and then turn on transcription,” Lim said. Once the T cells detect brevican, they activate a secondary program that expresses a “killing receptor”—a molecule designed to target and destroy tumor cells.
Precision targeting with two-factor authentication
Lim likens this multi-step process to two-factor authentication. The T cells require two specific signals to activate their killing function: the presence of brevican (indicating they are in the brain) and the identification of tumor-specific antigens. This dual requirement prevents the T cells from attacking healthy tissue outside the brain. “It’s like writing a program that says, ‘If in the brain, now kill this tumor,’” Lim explained. “We found that this worked really well…we could even implant the same tumor outside the brain, and the cells would leave that alone but clear the tumor in the mouse brain.”
Expanding the application: Beyond glioblastoma
The team believes this technique extends beyond glioblastoma. Lim’s team demonstrated that the system could target breast cancer metastases in the brain. “We can make a therapy based on this that attacks breast cancer metastases to the brain,” Lim noted, emphasizing its adaptability to different types of tumors. Additionally, the team explored using this “brain-sensing” circuit to produce anti-inflammatory molecules, offering a potential new avenue for treating neuroinflammation and autoimmune diseases like multiple sclerosis.
The engineered T cells have shown remarkable specificity and durability in preclinical trials. Lim highlights one of the study’s most exciting findings: “We re-challenged the mice. We took mice that were treated, cleared of their tumors, then re-injected a brain tumor…and they were able to clear it immediately.” This suggests the therapy could provide long-term immune memory, a key component for durable cancer treatment.
The next step is translating these findings into human trials. Lim’s team aims to initiate a clinical trial in 2025, focusing initially on glioblastoma and pediatric brain tumors. The modular nature of the “zip code” system also opens the door for applications in other organs and diseases. “We’re excited to think about whether we could design similar systems that recognize other organs in the body,” Lim said, envisioning a future where organ-specific targeting becomes a cornerstone of cellular therapy.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




