A new study led by researchers at the National Institutes of Health (NIH) has discovered that having just one genetic risk variant in the apolipoprotein L1 (APOL1) gene significantly increases the risk of developing kidney disease in people from West Africa. The study, conducted in collaboration with the Human Heredity and Health in Africa (H3Africa) Kidney Disease Research Network and published in the New England Journal of Medicine, says, specifically, these variants increase the risk of both chronic kidney disease and focal segmental apolipoprotein L1 (FSGS).
Prior research has established that genomic variants in APOL1 increase the risk of developing CKD among African Americans. However, limited data exists regarding how these variants impact individuals in West Africa, a region where many African Americans have genetic roots.
“Our study provides data about West Africans that will help us better understand the risk of chronic kidney disease associated with APOL1 variants,” said study co-author Adebowale A. Adeyemo, MD, deputy director of the Center for Research on Genomics and Global Health at NIH’s National Human Genome Research Institute (NHGRI). The intent of the research is to help develop risk assessments for kidney disease in populations with West African ancestry that could affect many Americans.
For their research, the investigators recruited more than 8,000 participants from Ghana and Nigeria—nearly 5,000 of whom were diagnosed with CKD and more than 800 who underwent kidney biopsies for confirmation of the disease. Their findings showed that nearly one-third (43% monoallelic APOL1 variants; 29.7% biallelic APOL1 variants) of the people from these two nations carry APOL1 variants that increased chronic kidney disease risk. An important finding was that having a risk variant in just one copy of APOL1 increases the risk of developing CKD, where previous studies among the African American population suggested that both copies of APOL1 needed to contain these variants to increase disease risk.
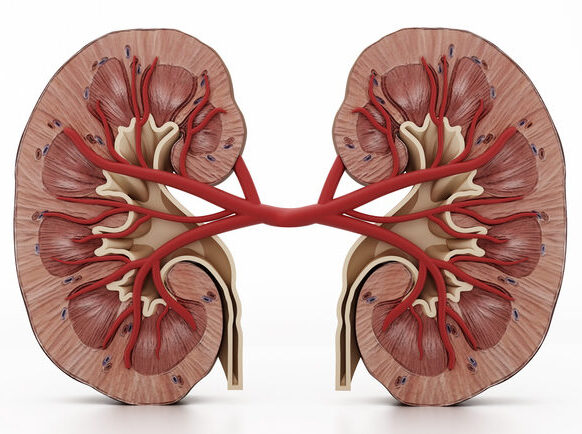
In addition to CKD, the presence of APOL1 variants dramatically raises the likelihood of developing FSGS, a rare kidney condition characterized by scarring of kidney tissues. Participants with two risk alleles showed an 84% higher risk of developing FSGS, while those with one variant had a 61% increased risk.
“Findings in a particular study or with a specific ancestral group are often taken to be true for all humankind, but there is often substantial diversity even within specific ancestry or ethnic groups,” Adeyemo stated. “This study highlights the importance of studying diverse populations around the globe when studying the genomics of human disease so that genomic medicine can equitably benefit people worldwide.”
Chronic kidney disease is a significant public health issue, affecting more than one-in-seven adults in the U.S. or roughly 37 million people. Higher prevalence rates are observed among African American, Hispanic American, and Native American populations, which may be influenced by both genetic predisposition and environmental factors. The complexity of kidney disease progression, often with few early symptoms, highlights the need for accurate early identification and intervention, particularly for individuals with comorbidities such as diabetes or hypertension.
“Further research conducted with participants in the United States can help us understand how APOL1 variants affect the kidney,” said Paul Kimmel, MD, program director at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and co-author of the study. “Overall, we hope that these findings can provide insight into improving the health of patients at risk for and with kidney disease.”
The implications of this study extend beyond West Africa, the researchers noted as other studies have also found APOL1 variants in populations from Europe, Asia, South American and Central America.





