A new study from researchers at the University of Cincinnati (UC) challenges the conventional view that newly approved monoclonal antibody Alzheimer’s drugs primarily work by clearing amyloid plaques. The research indicates that increases in a critical brain protein, rather than reductions in amyloid plaques, might be contributing to the slowing of cognitive decline in Alzheimer’s patients.
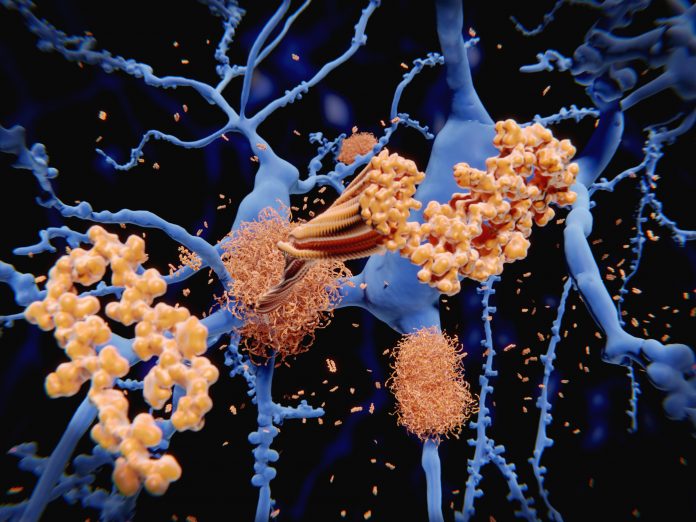
The study, published today in the journal Brain, questions the long-standing belief that a protein made up of 42 amino acids called amyloid-beta 42 (Aβ42) hardens in clumps called amyloid plaques that are the primary drivers of Alzheimer’s disease (AD) by damaging the brain.
Lead researcher Alberto Espay, MD, and his team at UC have hypothesized an alternate theory: that the normal soluble form of Aβ42 is essential for neuron health and that the loss of Aβ42, rather than plaque accumulation, might be the key factor in AD progression. This includes published research suggesting that dementia onset is not driven by high amyloid plaque levels, rather when Aβ42 levels are very low.
Espay’s hypothesis is that the buildup of amyloid plaques is a normal response to stressors in the brain, such as infections or metabolic changes. “Most of us will accrue amyloid plaques in our brains as we age, and yet very few of us with plaques go on to develop dementia,” said Espay who is a professor of neurology at the UC College of Medicine. “Yet the plaques remain the center of our attention in biomarker development and therapeutic strategies.”
The study investigated new monoclonal antibody medications that have been recently approved for their ability to reduce amyloid plaques. These drugs include aducanumab (Aduhelm) and lecanemab (Leqembi), which were developed for their plaque-clearing capabilities and have been shown to slow cognitive decline. Espay and his team discovered that these treatments also unintentionally increased levels of Aβ42 in the brain.
“Amyloid plaques don’t cause Alzheimer’s, but if the brain makes too much of it while defending against infections, toxins or biological changes, it can’t produce enough Aβ42, causing its levels to drop below a critical threshold,” Espay noted. “That’s when dementia symptoms emerge.”
For their study, the UC investigators analyzed data from nearly 26,000 patients who were part of 24 randomized clinical trials for new antibody treatments for AD. The researchers found that higher levels of Aβ42 following treatment were independently associated with slower cognitive impairment and less clinical decline.
“All stories have two sides—even the one we have told ourselves about how anti-amyloid treatments work: by lowering amyloid,” Espay said. “In fact, they also raise the levels of Aβ42. Even if this is unintended, it is why there may be a benefit. Our study shows that we can predict changes in cognitive outcomes in anti-amyloid trials at least as well by the increases in Aβ42 as by the decreases in amyloid.”
These findings align with Espay’s broader hypothesis that Alzheimer’s disease is more related to the loss of Aβ42 than to the presence of amyloid plaques. He argues that increasing Aβ42 levels, even if it means using treatments that also reduce amyloid, could be beneficial for cognitive function. “If the problem with Alzheimer’s is the loss of the normal protein, then increasing it should be beneficial, and this study showed that it is,” Espay said.
This research could also put clinicians in a difficult spot for treating patients, he noted, as removing amyloid from the brain is toxic and may cause the brain to shrink faster after antibody treatment. For this reason, Espay’s continuing research is focused on developing treatments that can increase Aβ42 levels without targeting amyloid plaques.





