
A research team funded by the National Institutes of Health (NIH) has developed a symptom-based scoring system that may help diagnose postacute sequelae of SARS-CoV-2 infection (PASC), or more commonly known as long COVID.
In a prospective observational cohort study of nearly 10 000 US adults, researchers found a total of 12 symptoms that contributed to the PASC scoring system. Findings also showed that PASC was more common and severe in participants infected before the Omicron variant emerged in 2021.
“A framework for identifying PASC cases based on symptoms is a first step to defining PASC as a new condition,” wrote investigators in the study published in JAMA. “These findings require iterative refinement that further incorporates clinical features to arrive at actionable definitions of PASC.”
The study is part of the NIH’s Researching COVID to Enhance Recovery (RECOVER) initiative, which aims to understand, treat, and prevent long COVID.
Defining PASC precisely can be difficult “because it is heterogeneous, composed of conditions with variable and potentially overlapping etiologies (eg, organ injury, viral persistence, immune dysregulation, autoimmunity, and gut dysbiosis),” wrote first author Tanayott Thaweethai, PhD, of Harvard Medical School in Boston, Massachusetts, and colleagues.
To better characterize PASC, Thaweethai and coworkers conducted an analysis of data from 9764 participants in the RECOVER adult cohort. The adult cohort consisted of adults with and without SARS-CoV-2 infection who were recruited from 85 sites across the US. Those who were enrolled before April 10, 2023, completed a symptom survey ≥6 months after acute symptom onset or test date, according to the study.
FINDINGS
Among the study cohort, 8646 (71% women, median age 47 years) tested positive for SARS-CoV-2 and 1118 tested negative.
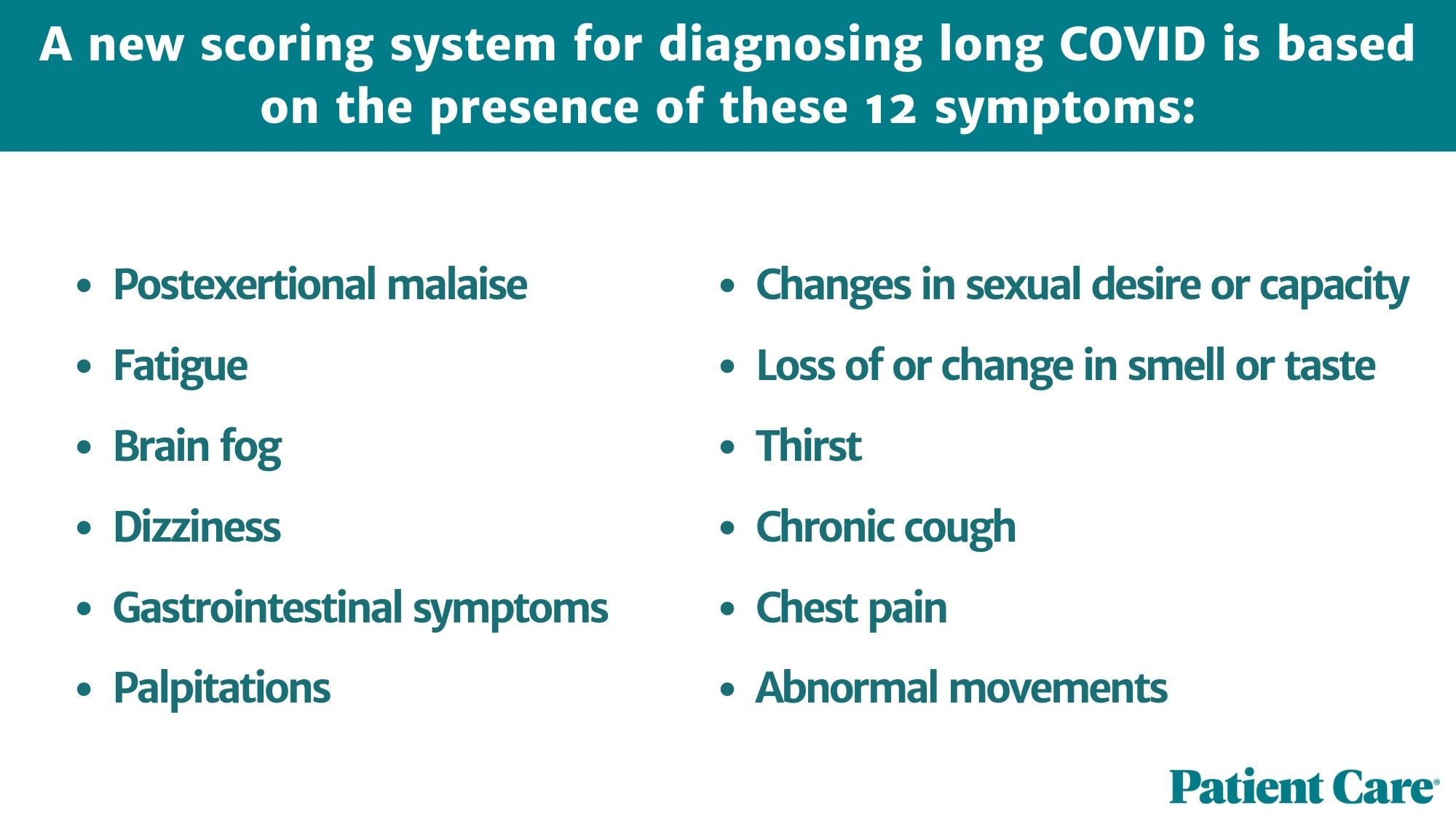
Overall, there were 37 symptoms with a frequency of ≥2.5% and adjusted odds ratios (ORs) were ≥1.5 (infected vs uninfected participants) for all 37, investigators observed. From these, they identified 12 symptoms that most set persons with PASC apart from those without PASC:
- Postexertional malaise
- Fatigue
- Brain fog
- Dizziness
- Gastrointestinal symptoms
- Palpitations
- Changes in sexual desire or capacity
- Loss of or change in smell or taste
- Thirst
- Chronic cough
- Chest pain
- Abnormal movements
The scoring system assigns scores to each of these 12 symptoms: 8 points for continued loss of smell or taste; 7 points for postexertional malaise; 4 points for chronic cough; 3 points for brain fog or thirst; 2 points for palpitations or chest pain; and 1 point each for fatigue, changes in sexual desire or capacity, dizziness, gastrointestinal symptoms, or abnormal movements.
Researchers established a threshold of 12 total points to identify participants with PASC. Based on this threshold, results showed that 10% (95% CI, 8.8%-11%) of the 2231 participants first infected on or after December 1, 2021, and enrolled in the study within 30 days of infection, were PASC-positive at 6 months.
“PASC positivity was more common and associated with more severe manifestation in participants infected in the pre-Omicron era,” added Thaweethai and coauthors.
A limitation to note of the current study is the fact that RECOVER recruitment is ongoing and not all study participants have reached the analysis stage.
“Definition of a classification rule for PASC requires an updated algorithm that incorporates symptoms as well as biological features,” concluded authors “Future analyses must consider the relationships among age, sex, race and ethnicity, social determinants of health, vaccination status after index date, comorbidities, and pregnancy status during infection on the risk of PASC and the distribution of PASC subgroups.”
Reference: Thaweethai T, Jolley SE, Karlson EW, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. Published online May 25, 2023. doi:10.1001/jama.2023.8823.









![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




