A study has revealed that coronary artery calcium (CAC) scores, which are determined via a CT scan, offer insights into the risk of developing coronary artery disease within five years and could change the rate at which statins are prescribed to patients. The research, conducted by researchers at Intermountain Health in Salt Lake City, suggests that a zero CAC score is not only a predictor of a low risk for coronary heart disease but that these people had a two to three times lower risk of death from any cause at any age.
The findings were presented at the American College of Cardiology’s annual scientific sessions last week.
“We found that a zero-plaque burden is not only highly prognostic of good heart health at any age, but also of excellent overall survival,” said Jeffrey L. Anderson, MD, principal investigator of the study. “Our findings show that having little or no coronary plaque predicts that people will live longer, healthier lives, including into their golden years.”
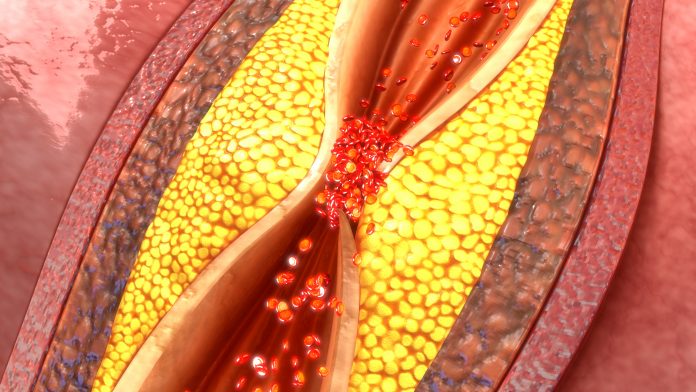
A coronary calcium CT scan uses X-rays to detect calcium deposits in the coronary arteries, a sign of plaque buildup. This imaging method allows doctors to detect plaque before it leads to more serious conditions like heart attacks, offering a more proactive approach to treating heart disease. A coronary artery calcium score of zero indicates essentially no advanced coronary plaques; a score of 1–99 indicates a mild case of plaque; a score of 100–299 a moderate case: and a score of 300 or more a high case. Anderson noted that the risk of a coronary event in the overall population generally parallels the calcium plaque found in the arteries.
The retrospective study, part of the CorCal Outcomes trial, involves 40,820 symptomatic patients over a span of 10 years who were at risk at primary coronary risk. These patients underwent a PET/CT scan, which has the ability to quantify advanced calcified plaque in heart vessels.
The data showed that patients with a CAC score of zero experienced coronary events at a very low rate: only 0.12% in younger patients and 0.25% in patients older than 65.
The investigators also indicated the levels of coronary artery calcium could indicate the relative health of organs beyond the heart. “If you have disease in your coronary arteries, you may also have vascular complications in other organs of your body,” said Anderson. “Given these results, a zero coronary artery calcium score may also be a predictor of not only very low coronary death but also of a lower risk of other causes of death.”
In addition to helping to determine high-risk coronary patients, CorCal also has the potential to more effectively guide decisions about prescribing the cholesterol lowering drugs statins. Statins are commonly prescribed based on traditional risk-scoring methods such as the Pooled Cohort Equations (PCE), which assess risk based on factors like age, sex, cholesterol levels, and smoking status. However, using a CT scan to determine the presence of coronary artery calcium may offer a more personalized and accurate approach to statin prescription. “The question is: Can we do a better job in selecting people who need a statin for primary coronary risk reduction by using the coronary artery calcium score?” Anderson said at the American College of Cardiology’s annual scientific sessions.
For this portion of the study, the researchers sought to discover the differences in statin prescribing when using the PCE versus CAC scores. In the study, 50.7% of patients in the PCE group were recommended statins, while only 22.3% in the CAC group received such a recommendation. This significant difference is mainly due to the influence of older age in the PCE, which often results in statin recommendations for patients who may not have coronary artery disease. On the other hand, many older patients in the CAC group had zero or low scores, leading to fewer statin prescriptions.
The CorCal Outcomes study is expected to conclude in 2026. Over the next few years, the researchers will continue to compare outcomes such as heart attacks, strokes, and death rates in both statin groups to assess which method of prescribing statins provides the best results for patients. “We know there’s a huge difference in prescribing recommendations, and next year we are anxious to see the impact of these differences on outcomes,” Anderson said.
The findings have the potential to influence clinical decisions. Knowing a patient’s coronary calcium score could help identify people who are at greater risk of heart disease and those who could benefit from early interventions. It also has the potential to reduce unnecessary prescriptions, avoiding the side effects and costs associated with statins for those who do not need them.
The researchers also plan to further investigate how a zero CAC score correlates with overall health outcomes, particularly in relation to vascular diseases in other organs and possibly even cancer.








![Best Weight Loss Supplements [2022-23] New Reports!](https://technologytangle.com/wp-content/uploads/2022/12/p1-1170962-1670840878.png)




