Research led by the Cleveland Clinic has identified specific groups of microglia linked to Alzheimer’s disease as well as the genes driving the disease transition.
The investigators also identified that use of the non-steroidal anti-inflammatory drug (NSAID) ketorolac, which is already approved by the FDA, could help reduce the incidence of the condition.
Alzheimer’s disease is a neurodegenerative disease of aging that impacts around 6.7 million people over the age of 65 years in the U.S.
“Lecanemab (Leqembi) and donanemab (Kisunla), monoclonal antibodies targeting aggregated amyloid, were recently approved as the first disease-modifying medicines for early Alzheimer’s disease patients,” wrote Feixiong Cheng, PhD, a principal investigator at the Cleveland Clinic, and colleagues in the journal Alzheimer’s & Dementia.
“However, anti-amyloid drugs are unlikely to act after symptom onset and potential side effects and high cost may limit their use in broad Alzheimer’s disease populations. Without effective disease-modifying treatments, this represents an unprecedented crisis of human suffering and financial cost.”
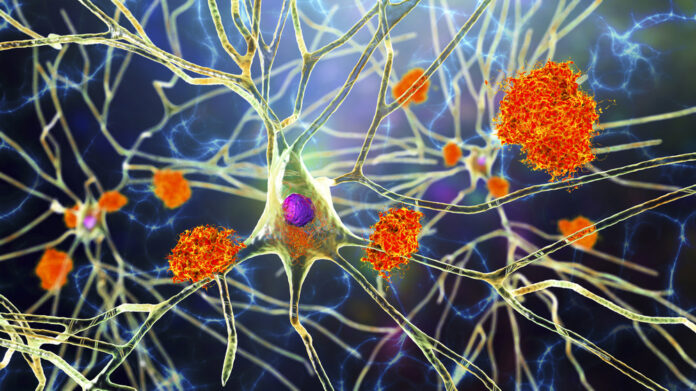
Microglia are immune cells that normally help protect the immune system and keep it free of pathogens like viruses and bacteria. However, abnormal microglia can form that contribute to the progress of Alzheimer’s.
In this study, Cheng and team used a specific type of artificial neural network to analyze 700,000 single-cell RNA transcriptomes from human brains and evaluated links between disease-associated microglia and Alzheimer’s.
The researchers identified that the genes SYK, CTSB, and INPP5D were linked to the abnormal transition to disease-associated microglia, tau microglia, and neuroinflammation-like microglia. They then looked at drugs that might have a beneficial influence on this transition.
Using two real-world patient databases, Cheng and colleagues showed that use of the NSAID ketorolac was linked to an 11–17% reduced incidence of Alzheimer’s in the two cohorts. They showed it downregulated Type-I interferon signaling in microglia, which they think is behind its protective effect.
“Microglia have been implicated in Alzheimer’s disease for over a century. So far, attempts to stop disease progression with broad spectrum anti-inflammatory drugs and ‘harmful’ microglial blockers have been ineffective. We need to selectively block harmful microglia subtypes while leaving normal, healthy microglia intact,” said Cheng in a press statement.
“Our study offers a powerful deep generative model to identify repurposable drugs from many types of Alzheimer’s disease findings, but the overall methods can be broadly applied to other diseases as well.”
The team now plans to evaluate its findings further and carry out additional studies to verify the effects of ketorolac in Alzheimer’s disease progression.





