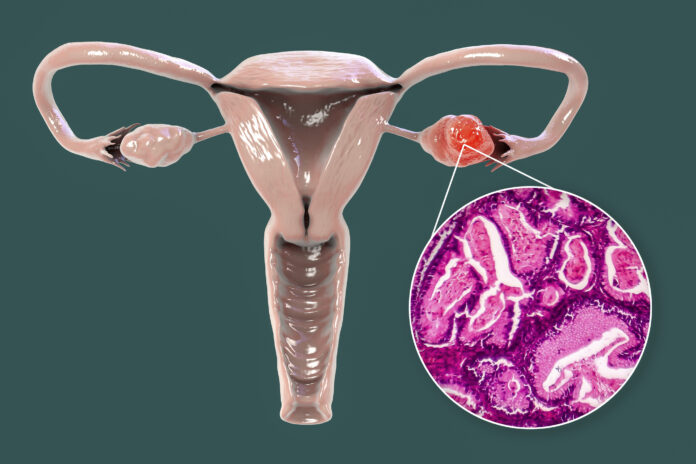
Using spatial genomics technology, studies in preclinical animal models, and evaluation of tumor specimens from ovarian cancer (OvCa) patients, scientists at the Icahn School of Medicine at Mount Sinai discovered ovarian cancer tumors produce interleukin-4 (IL-4)—which is typically associated with asthma and the skin condition eczema—to produce a protective tumor microenvironment to resist immunotherapy.
The findings published in Cell point to a potential drug target that could overcome immunotherapy resistance, and also to the potential to repurpose an IL-4 blocking drug that is FDA-approved for treating asthma and eczema, to enhance immunotherapy for ovarian cancer.
The research was led by Alessia Baccarini, PhD, assistant professor of immunology and immunotherapy, and Brian D. Brown, PhD, director of the Icahn Genomics Institute at Icahn Mount Sinai. In their paper, the team said their findings “… reveal OvCa-derived IL-4 is a key switch in establishing the immunosuppressed ovarian TME and suggest blocking IL-4 signaling may improve the response to immunotherapy in OvCa.”
Ovarian cancer is one of the most deadly cancers, with a five-year survival rate of less than 50%, the authors wrote. While immunotherapy drugs such as pembrolizumab, which targets the PD-1 molecule, have demonstrated efficacy in treating melanoma and lung cancer, they have not significantly improved survival rates in ovarian cancer. “Although immunotherapies, specifically immune checkpoint blockade (ICB) targeting PD-1/PDL1 signaling, have been effective for many cancers, in OvCa, ICB has shown limited clinical benefit, with objective response rates
This is partly because ovarian tumors have fewer mutations, making them harder for the immune system to recognize. Additionally, research suggests that these tumors may resist immunotherapy by creating barriers that prevent immune cells from infiltrating their borders. “The ovarian tumor microenvironment (TME) is commonly in an immune-suppressed state with local exclusion and/or suppression of T cells, which is considered a contributing factor to the poor ICB response,” the team stated. The critical question, they noted, has been, how do tumors establish these protective environments?
To address this question, Brown, Baccarini, and colleagues harnessed Perturb-map, a novel spatial functional genomics technology. Perturb-map enhances traditional gene-editing CRISPR screening—where hundreds of genes are simultaneously “perturbed”—by incorporating state-of-the-art spatial imaging.
This enables each gene’s role in controlling the tumor environment to be elucidated. “To identify regulators of ovarian cancer immunity, we employed a spatial functional genomics screen (Perturb-map), focused on receptor/ligands hypothesized to be involved in tumor-macrophage communication,” they explained.
Their experiments revealed that removing the IL-4 gene from ovarian cancer cells rendered the tumors susceptible to anti-PD-1 therapy. “Surprisingly, the IL-4-deficient cancer cells were eliminated by the immune system even when mixed within tumors containing IL-4-producing cancer cells, a phenomenon known as intratumoral heterogeneity, which also contributes to drug resistance in cancer,” noted senior author Brown, who is also a Mount Sinai professor of genetic engineering.” The authors further stated, “Perturb-map recapitulated tumor heterogeneity and revealed that interleukin-4 (IL-4) promotes resistance to anti-PD-1 … IL-4 loss was not compensated by nearby IL-4-expressing clones, revealing short-range regulation of TME composition dictating tumor evolution.
The researchers then tested a combination of anti-PD-1 and IL-4 receptor-blocking drugs in mice with aggressive metastatic ovarian cancer and found that this combination treatment significantly extended survival.
Additional preclinical studies demonstrated that ovarian cancer uses IL-4 to program macrophages, a type of immune cell, into protectors of the cancer cells. The IL-4-programmed macrophages prevented T cells from killing the cancer cells. However, when IL-4 was blocked, the local environment surrounding the cancer cells changed, and this left the malignant cells susceptible to being eliminated by the immune system. “Notably, we identify IL-4 as a key factor in promoting ovarian tumor resistance to ICB and show that, although produced by only a small fraction of OvCa cells at any time, IL-4 has a significant impact on programming the TME,” the investigators wrote. “We further demonstrate OvCa cells are the key source of IL-4 in ovarian tumors and that combining PD-1 and IL-4 receptor (IL4R) blockade converts anti-PD-1 non-responsive tumors to responsive,” they noted.
To further validate their findings, the team examined specimens from human ovarian tumor resections and saw that the patients’ cancer cells also produced IL-4. Moreover, analysis of single-cell RNA sequencing data from patient tumors—which examines how genes are expressed in cells—revealed that the macrophages displayed a strong IL-4 signature, suggesting that IL-4 is playing a similar role in human ovarian cancer and may be one of the reasons patients have not benefited from immunotherapy.
“Ovarian cancer has almost been written off as non-responsive to existing immunotherapy, so it was quite stunning to us that by just blocking this one molecule, IL-4, and altering the tumor’s microenvironment, we could make these difficult-to-treat tumors more treatable,” added Brown. “This is further evidence that targeting the tumor’s neighborhood, not just the cancer cells, can be beneficial.”
While these findings are encouraging, the investigators stress that clinical trials are essential to determine whether targeting IL-4 can enhance patient outcomes. Given that dupilumab is already FDA-approved for asthma and eczema, there is potential for swift clinical testing alongside immunotherapy to enhance survival in ovarian cancer patients. Thomas Marron, MD, PhD, director of the Early Phase Trial Unit at Mount Sinai and a colleague of Brown and Baccarini, has already been running a clinical study to test whether dupilumab can improve anti-PD-1 immunotherapy in patients with lung cancer, and several patients have shown beneficial responses. “Our studies, implicating IL-4 as a mechanism of anti-PD1 resistance and the synergistic therapeutic benefit of anti-PD-1 and anti-IL-4R, suggest OvCa may also be a good candidate for combined PD1 and IL4R blockade,” the team noted in their paper.
The IL-4 pathway is already targeted for diseases like eczema, so the researchers are hopeful it can help them now target ovarian cancer. The findings may lead to new strategies and therapeutics for a cancer that is difficult to diagnose early.

![Histological image of an ovarian cancer patient’s tumor analyzed for IL-4. Cancer cells expressing the gene PAX8 (green) also show IL-4 expression (red), which was found to help protect the cancer cells from the immune system. [Mollaoglu et al., Cell]](https://www.genengnews.com/wp-content/uploads/2024/10/low-res-11-300x78.jpeg)




