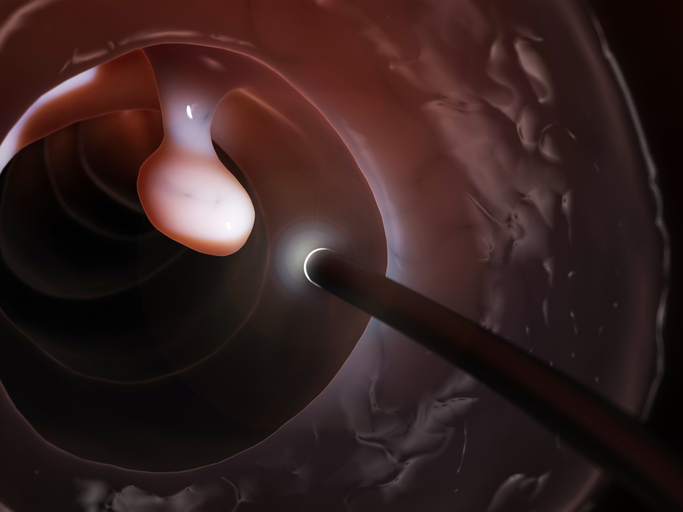
Colonoscopy remains the cornerstone for colorectal cancer (CRC) screening, with adenoma detection rate (ADR) being a crucial quality metric. However, detecting adenomas during colonoscopy is challenging due to human error, leading to the development of computer-aided detection (CADe) systems that use artificial intelligence (AI) to assist endoscopists in identifying polyps.
A new systematic review and meta-analysis in Annals of Internal Medicine revealed the ADR was significantly higher with CADe systems—44.7% versus 36.7% in conventional colonoscopy. This 21% increase is consistent with previous studies that suggest CADe’s ability to help clinicians identify polyps that might otherwise be missed. The study included data from 44 randomized controlled trials comprising over 36,000 cases, offering one of the most comprehensive evaluations of CADe systems in colonoscopy to date.
Adenoma detection: CADe outperforms conventional colonoscopy
The primary outcome of interest in the review was the average number of adenomas detected per colonoscopy (APC). The data shows a clear advantage for CADe-enhanced colonoscopies, with an average APC of 0.98 compared to 0.78 for conventional methods. The study suggests that for every 10 colonoscopies, two more adenomas are detected when using CADe.
In contrast, the adenoma miss rate (AMR), the rate at which adenomas are missed during colonoscopy, also showed a marked reduction in CADe-enhanced procedures. The use of CADe resulted in a nearly 60% reduction in AMR.
An uncertain impact on advanced colorectal neoplasia detection
Despite the clear benefits in adenoma detection, the effect of CADe systems on detecting more clinically significant lesions, such as advanced colorectal neoplasia (ACN), remains ambiguous. The average ACN per colonoscopy was similar between CADe and conventional methods. However, the detection rate for ACN was slightly higher with CADe (12.7% vs. 11.5%, RR = 1.16), indicating a 16% increase in the detection rate for these advanced lesions.
The authors believe the mixed results for ACN detection can be attributed to the heterogeneous nature of the studies included in the analysis. While CADe systems consistently boost ADR and APC, their impact on the detection of more advanced, potentially cancerous lesions may depend on various factors, such as the patient population and the specific CADe platform used.
Balancing benefits with procedure time and nonneoplastic polyp resection
The authors observed one downside to the use of CADe systems; a small but statistically significant increase in procedure time. Withdrawal time, the period during which the endoscopist carefully inspects the colon for polyps while removing the scope, was extended by an average of 0.53 minutes in CADe-enhanced procedures. Although this time increase is relatively modest, it may be a consideration in high-volume clinical settings where efficiency is critical.
Another potential drawback is the increased resection of nonneoplastic polyps (NNPs). The use of CADe resulted in the removal of nearly two extra NNPs per 10 colonoscopies. While removing NNPs is not harmful, unnecessary resections can lead to additional biopsies and associated costs without providing significant clinical benefit. This highlights the need for CADe systems to improve their specificity in distinguishing between neoplastic and nonneoplastic lesions.
Variability in results: The role of neural network architecture and study limitations
A notable aspect of the review is the lack of clear differences in performance between different CADe systems based on their underlying neural network architectures. Deep learning systems used in CADe vary widely in their design and training, yet the review found no significant difference in efficacy among them. This suggests that while CADe systems are generally effective at enhancing adenoma detection, the specific choice of AI platform may be less important than ensuring proper integration into clinical workflows.
The review also acknowledges several limitations in the included trials. One key challenge is the inability to blind endoscopists to the use of CADe systems. This could introduce a Hawthorne effect, where clinicians alter their behavior simply because they know they are being observed, potentially inflating ADRs in both the CADe and control groups.
Additionally, the heterogeneity among studies in terms of patient population, CADe platforms, and procedural factors (e.g., withdrawal time) complicates the interpretation of the results. The authors caution that further research is needed to better understand the interactions between these factors.
Clinical implications: Who benefits most from CADe?
Despite the limitations, the review provides valuable insights into which patient populations may benefit most from CADe-enhanced colonoscopies. Notably, the benefit of CADe systems appears to be reduced in patients with a positive fecal immunochemical test (FIT), which is often used as a preliminary screening tool for CRC. This suggests that CADe may be more useful in general screening populations rather than in individuals who have already been flagged as high-risk by a FIT.









