As a graduate student at the Weizmann Institute studying systems biology, Eran Eden frequently found himself with a peer, Kfir Oved, an MD-PhD candidate at the time, playing a “game” in the evenings in their grandmothers’ kitchens while eating blintzes, a classic of Eastern European cuisine.
The “game” they played over plates with these rolled pancakes stuffed with, in this case, savory mushrooms—blintzes are also often stuffed with sweet cheese and jam for dessert—didn’t involve cards or dice.. Instead, grandma’s cooking fueled the quintessential scientist’s pastime of identifying and solving a problem that would change the course of history.
But after a year, many blintzes were eaten, but ideas didn’t materialize. “You hear about people coming up with an idea over dinner and then going to execute it, but for us, it was just darkness—nothing,” Eden told Inside Precision Medicine.
But one day, Eden and Oved started to zero in on an issue that’s pretty common, even universal, when catching an infection, figuring out if the underlying cause of illness is bacterial or viral, thereby empowering clinicians, parents, and patients to make better-informed decisions regarding whether to treat a particular infection with antibiotics or none at all.
“I have three young kids, little incubators of bacteria and viruses, and, on a bi-quarterly basis…it comes down to whether to treat them with antibiotics in case of bacterial infection or chicken noodle soup in case its a virus,” Eden said. “And it’s not just our kids—we and our parents, too. It’s probably one of the most prevalent things we encounter. It’s a pretty big riddle for providers and the healthcare system as a whole.”
So, when Eden and Oved finished training, they postponed their academic careers to pursue this diagnostic problem. One month became a quarter, a quarter became a year, and a year became more than a decade. Sometime during the beginning, they started a business called MeMed with Eden as CEO and Oved as CTO, where they began to develop an in vitro diagnostic (IVD) test and a point-of-need platform called MeMed BV and MeMed Key, respectively, to help solve whether to use penicillin or split pea soup.
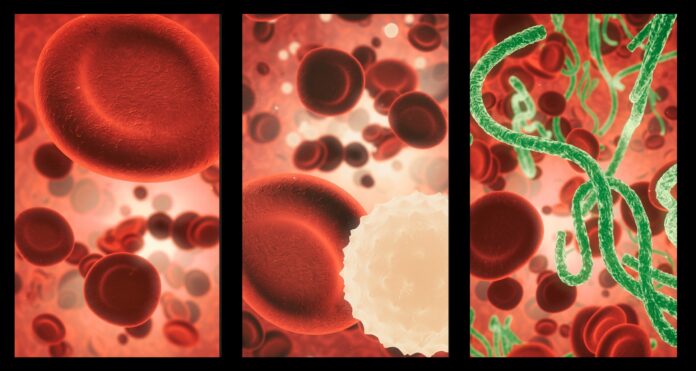
Since then, they’ve improved their assay to accurately distinguish between bacterial and viral infections in just 15 minutes using a 100-microliter blood sample. MeMed received the CE-IVD mark in June 2020 for using the MeMed BV test on the MeMed Key platform to distinguish between bacterial and viral infections in Europe, and the FDA granted 510(k) clearance in September 2021.
Since then, MeMed has been working to prove the use of its approach to improve patient outcomes and optimize healthcare decision-making. Today, MeMed announced that its first pilot randomized controlled trial to evaluate the MeMed BV test in the US has been completed, successfully demonstrating clinical utility in promoting appropriate antibiotic use.
“It’s the first time that the results of a randomized control trial on an advanced host response technology have been provided,” said Eden. This achievement is critical to making MeMed BV the standard for distinguishing bacterial from viral infections and advancing efforts to expand reimbursement coverage.
The JUNO trial, named after the NASA space program orbiting Jupiter, was conducted across 11 emergency departments (EDs) and Urgent Care Centers (UCs) in the US and Israel. It enrolled 260 adult patients with clinical suspicion of lower respiratory tract infection (LRTI).
Some of the results are very encouraging, including the finding that in cases where antibiotics were potentially unwarranted, antibiotic prescription rates were 33% in the control group versus 13% in the MeMed BV group, representing a 62% relative reduction. Importantly, EDs or UCs revisits were similar between the control group and the MeMed BV interventional group despite the significant decrease in antibiotic prescriptions.
Nature’s cheat code
Returning to the original clinical scenario of a sick person going to a clinic, emergency department, or urgent care facility is crucial to grasping MeMed’s approach and possible relevance. In most cases, patients leave without having learned much about their condition, despite the use of what Eden terms “clinical gestalt” and possibly a pathogen detection test (the latter of which used a giant Q-tip to swab the inside of a person’s throat to obtain a sample to grow in a culture). Even with the increasing use of PCR and antigen testing following the SARS-CoV-2 pandemic for viruses like influenza, these methods have flaws, as with any diagnostic.
There’s a significant limitation when it comes to getting samples: they are limited to identifying pathogens in select sites in the body. While Q-tips can reach way up into the nostril, many infections sites are simply inaccessible or unknown. No one will puncture the tympanic membrane to get a sample for an ear infection, and it’s difficult to reach into the lungs to test for things like pneumonia that may not come up in a sputum culture. And how will any sample provide a readout of potential infection sites in the body, including the brain, heart, and pancreas?
Additionally, many diagnostics are only sensitive to specific periods of the infection, as some need to be taken at infection onset, and others will be missed early on. For example, antibody tests may appear falsely negative during the first few weeks of infection, typically when a patient has an erythema migrans rash, but FDA-cleared assays have suitable sensitivity after 4-6 weeks have passed.
Another temporal issue is the time to results, which, for many of the existing technologies, typically takes anywhere from half a day to 48 hours, depending on whether it requires growing a culture, which is another process that can fail. Then there’s the ease-of-use factor—not everyone can run a PCR, but everyone knows how to use a basic lateral flow test. All these issues together lead to antibiotic misuse, operational inefficiencies, and patients who don’t get better, leading to a slew of massive healthcare and economic problems.
So, for MeMed team, it was important to develop an easy-to-use technology that could quickly and accurately detect an infection anywhere in the body. The solution MeMed came up with involves understanding the host immune response rather than directly identifying the pathogen. In fact, according to Eden, they “cheated.”
“Rather than attempting to detect the [individual pathogens], we decided to use the best detection system available, far superior to anything we could ever hope to develop as scientists, clinicians, or engineers, and I am referring to your immune response or immune system, which is arguably the ideal machinery for detecting bacterial viruses and launching specific attacks against them,” said Eden. “You might not always detect the pathogen, but the immune system is waging the war. So it’s always going to give you the results.”
MeMed developed machine learning and computational algorithms to determine if the body fights viruses or bacteria and at what stage the host immune system functions. This led them to three host immune proteins: TNF-related apoptosis-induced ligand (TRAIL), interferon γ-induced protein-10 (IP-10), and C-reactive protein (CRP).
“What’s interesting about the biomarkers that we found and use in cooperating signatures is that they have different temporal dynamics,” said Eden. “For example, one of the proteins in our signature is a protein called TRAIL that shoots up in your bloodstream in the pre-symptomatic stage, meaning that when you come to the doctor with your kid, it’s already highly elevated. So, you can show a pretty robust response, irrespective of when symptoms onset. This technology works on early and late infections because you collect different information from different biomarkers; none of them is sufficiently accurate in itself but, as a team, they provide a pretty accurate and robust result.”
Antimicrobial resistance and health inequality
Where MeMed’s approach falls short is in providing the resolution needed to narrow down the type of antibiotic best suited for an infection. However, that doesn’t make it useless—far from it. Just the ability to detect whether an infection is bacterial or viral is a huge step toward addressing the growing global health threat of antimicrobial resistance.
“The host response, at least the first layer, tells you bacteria versus viral, to treat or not treat, which is a big part of the problem,” said Eden. “If you could just remove all the cases where antibiotics are prescribed to a viral infection for which they’re ineffective, you would solve a big portion of the problem.”
One in five patients does not receive antibiotics on time, even though they could benefit from them. Another problem is overprescribing antibiotics for infections that are not bacterial.
“We can potentially reduce both the overuse of antibiotics and the underuse, so you’re both reducing inappropriate overuse, thereby addressing this issue of antimicrobial resistance (AMR) and other elements such as adverse events and as a result of antibiotics, but equally important, you’re also catching cases, that could benefit from antibiotics and are not receiving treatments.”
Eden equates AMR to global warming, not just in potential scale of impact but also in terms of short-term relief—in the case of global warming, it’s the overuse of fossil fuels and the ease and immediacy of the impact on giving us quick ways to move about, regulate temperature, and produce and ship all sorts of products seemingly on-demand. Similarly, if prescribing antibiotics might get a screaming child to get better and a doctor wants to play it safe rather than sorry by wishing to avoid potential sepsis, then why not prescribe antibiotics?
In addition to AMR, MeMed hopes to improve healthcare equity. As Eden described, MeMed’s approach has the potential to address variables that make care geographically accessible and affordable to all people by providing an inexpensive, simple benchtop solution.
The solution also addresses another challenge to healthcare inequality, and that’s how treatment may differ between being able to see a doctor during the middle of a work day or in the middle of the night on the weekend. “There’s a joke that if you want to be sick, go to the ED during the day when you get the doctor, not the intern at night,” said Eden. “MeMed can help with care equity—everybody gets the same test quality and result.”
So, while MeMed will lose out to approaches such as the Karius test, a centralized metagenomics approach that can identify pathogens in the blood using cell-free DNA (cfDNA) when it comes to explicitly identifying microbes, it holds a heavy advantage when it comes to diagnosing inaccessible infections, rapid time to results and accessibility worldwide with a point-of-need platform.
Eden sees these different tools as complementary. In some situations, such as with a critically ill patient who could go into septic shock, nailing down the sub-strain of a pathogen will be important. However, that scenario is far less common than what Eden and Oved set out to do over 13 years ago as graduate students hanging out at a table in grandma’s kitchen.