UCLA Health Jonsson Comprehensive Cancer Center researchers have used a platform-based method to create the largest collection of personalized organoid models for patients with sarcoma to date.
If confirmed through clinical trials, the predictive power of the platform “could help make data-driven decisions, so that the therapy with the highest chance of success is chosen for each specific patient,” said Alice Soragni, PhD, senior author of the study and assistant professor in the department of Orthopedic Surgery at the David Geffen School of Medicine at UCLA.
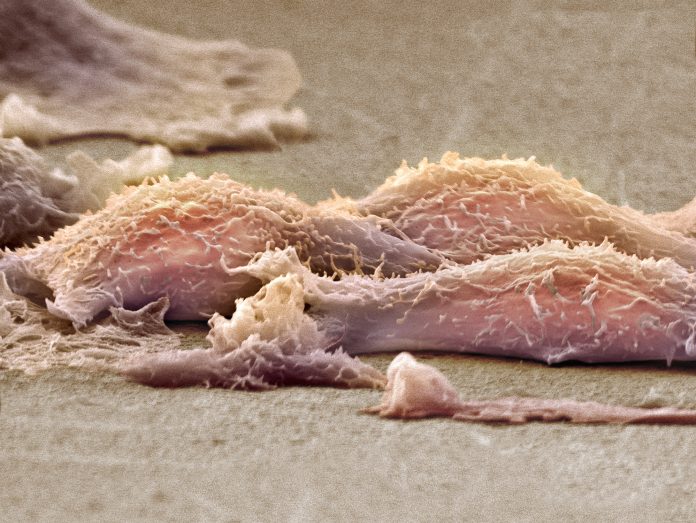
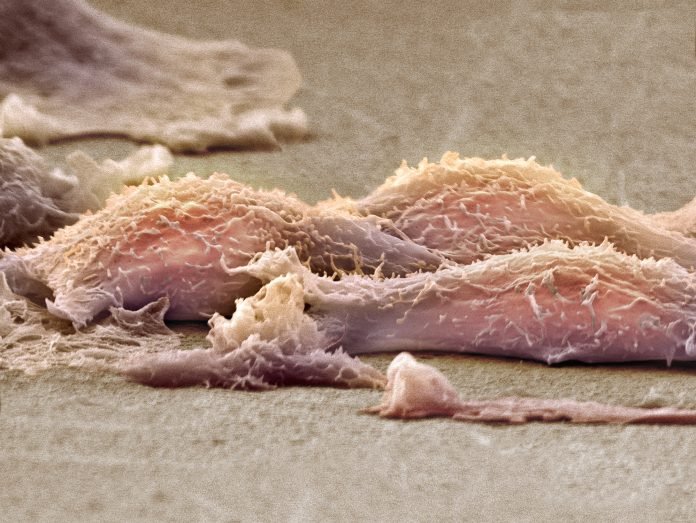
Sarcoma is a rare cancer with limited treatment options and poor outcomes. With over 100 distinct and heterogeneous tumor types arising from bone, connective, and soft tissues there are few, if any, patient-derived models available to study disease biology, identify new therapies, or personalize treatment approaches, Soragni explained.
“Recognizing this gap, we saw an opportunity to leverage the expertise of the UCLA Sarcoma program, one of the largest in the country,” she said. “We worked very closely with the team, which includes sarcoma pathologists, surgeons, oncologists, and radiation oncologists, to develop patient-derived organoid models of sarcoma, and use these to advance sarcoma research and precision medicine.”
Soragni and team collected 194 tumor samples from 126 UCLA patients diagnosed with 24 different subtypes of bone and soft tissue sarcoma. While tumor organoids have been widely used to study carcinomas, this study is the first of its scale to extend organoid development to sarcoma.
They successfully created patient-derived tumor organoids from 114 samples encompassing 21 different sarcoma diagnoses and conducted detailed histopathological and molecular analyses to confirm that the organoids retained key characteristics of the original tumors.
The organoids were then subjected to high-throughput drug screening using a mini-ring pipeline developed by Soragni and her team. On average, 117 drugs were tested per sample, with the screening panel tailored to individual characteristics, histology, patient-specific data, and clinical background. The researchers note that their selection criteria focused on FDA-approved therapies and National Comprehensive Cancer Network (NCCN)-recommended combination regimens for each sarcoma subtype but also included drugs targeting genetic alterations identified in the samples.
Results of these medium-to-large scale screenings on 3D tumor organoids were available within a week from surgery, in the researchers’ report in Cell Stem Cell.
“Time is critical when the goal is treatment prediction and eventually guidance,” said Soragni. “We have worked diligently to establish a workflow from the operating room to the lab, and developed standardized organoid culture conditions that preserve the unique histopathological and molecular features of the tumor of origin.”
She added that the optimized tissue handling and freezing protocols they developed will allow them to receive high-quality tissue from external partners. “Thus, with the right infrastructure and coordination, large-scale implementation of organoid-based programs is not only feasible but can be extended across institutions.”
In the current study, the method identified at least one potentially effective FDA-approved or NCCN-recommended regimen for 59% of the specimens, demonstrating the potential of the pipeline to provide actionable treatment information.
“However, while these drugs are approved for cancer, only a small portion is approved specifically for the cancer type they are effective against,” cautioned Soragni. This raises the issue of off-label access, but Soragni says that if the predictive power of organoids can be validated in clinical trials, it is possible that the data “could pave the way for broader or more flexible [drug] use in the future, particularly for rare or difficult-to-treat cancers.”
The investigators also showed that the drug responses observed in the organoids matched how the patients responded to treatment for a small number of cases, suggesting that these organoids could be a powerful tool for guiding clinical decisions.
They have recently initiated PREMOST: a PREcision Medicine trial in OSTeosarcoma. A 40-patient trial that will systematically evaluate the feasibility of the mini-ring patient derived organoid platform to predict responses to neoadjuvant therapy in patients with newly diagnosed osteosarcoma. The team will also investigate second-line therapies for recurrent and metastatic osteosarcoma, with an opportunity to return results to the clinic. “While the treatment decision is up to the oncologist, we will evaluate how our results impact that choice, and ultimately compare the responses in organoids to clinical outcomes,” said Soragni.
She believes that in an ideal world, organoids should be generated for all patients, ideally as early as possible. “Tumor evolution and heterogeneity can make it challenging to stay ahead in predicting responses and generating organoids early can provide a more representative picture.”