Research in human cells and in mice by scientists at the Johns Hopkins Kimmel Cancer Center suggests that age-related changes in fibroblasts contribute to the development of aggressive, treatment-resistant melanoma in males. The researchers, co-led by Ashani Weeraratna, PhD, the Bloomberg Distinguished Professor, E.V. McCollum Professor, and chair of the department of biochemistry and molecular biology at Johns Hopkins, discovered that human skin fibroblasts—cells that create the skin’s structure—show age-and sex-specific changes in proliferation and stress response, and that male fibroblasts age faster due to elevated levels of reactive oxygen species (ROS).
The studies in addition indicated that bone morphogenetic protein 2 (BMP2) is secreted in the aged male dermal microenvironment, and this promotes invasive melanoma that is resistant to BRAF/MEK inhibition. Further investigation showed that inhibiting BMP2 activity blocked development of this invasive tumor phenotypes and sensitized the melanoma cells to BRAF/MEK inhibition.
The findings were published in Cell.
The risk of developing melanoma, a potentially deadly skin cancer, increases with age. “Older patients (>55 years) account for 40% of melanoma diagnoses, often diagnosed at advanced stages, with decreased melanoma-specific survival compared with younger patients,” the authors wrote. Men are more at risk than women, and tend to develop more aggressive, hard-to-treat melanomas, particularly at advanced ages, said Weeraratna. However, why this sex-related difference exists isn’t known. “In cutaneous melanoma, the underlying biological mechanisms responsible for sex disparity are unknown and complicated by clinical variables such as anatomical site, skin phototype, body mass index, and variability in immune responses,” the authors pointed out.
Weeraratna and colleagues have demonstrated that age-related changes in the normal cells in the tumor microenvironment (TME)—contribute to cancer outcomes. Fibroblasts make collagen, a protein that gives the skin structure and strength. In previous research, Weeraratna and colleagues showed that age-related changes in fibroblasts promote the spread of melanoma tumor cells and lead to worse outcomes. “Previous work from our laboratory has shown that aged dermal fibroblasts promote a ‘‘phenotype switch’’ in melanoma cells …” they stated. “We previously demonstrated that aging microenvironments promote melanoma invasion and metastasis as a result of altered fibroblast secretomes, and these changes contribute to inferior age-dependent clinical outcomes.” However, they added, “… we did not assess the effects of sex … understanding the fundamental differences in molecular circuitry between a male vs. female tumor microenvironment (TME) is warranted to determine the underlying molecular basis of melanoma progression and therapy resistance.”
The authors wanted to find out if age- and sex-related changes might interact to contribute to sex-linked disparities in melanoma. “Melanoma is far more aggressive in men than women,” Weeraratna continued. “Do normal cells around the tumors age differently in men versus women?”
The scientists’ newly reported studies, including an analysis of fibroblasts from human male and female melanoma patients of different ages, confirm that fibroblasts age differently in men and women, and that the age-related changes occurring in male fibroblasts contribute to more aggressive, hard-to-treat melanomas. When the investigators transplanted melanoma tumor cells into aged male or female mice, they found more DNA damage accumulated in cells transplanted in the male mice. Interestingly, it didn’t matter whether the transplanted tumor cells came from male or from female mice.
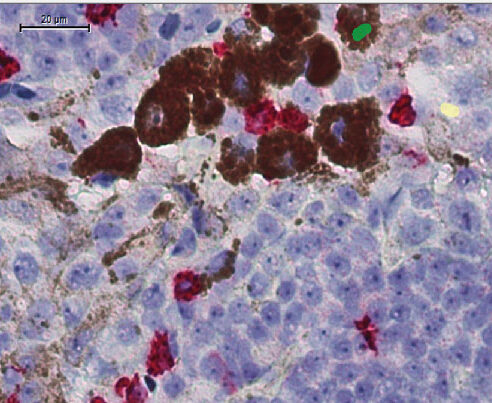
“It’s not the male or female tumor cell itself,” Weeraratna explained. “Age-related changes in male fibroblasts that make up the tumor microenvironment account for differences in DNA damage.” In experiments comparing aged human male and female fibroblasts, the team discovered that the male fibroblasts accumulated reactive oxygen species that stress and damage cells. Reporting on analyses, they stated, “These data suggest that stromal cells in the aged male TME induce more oxidative stress in melanoma tumors relative to the female TME.” They also found that the aged male fibroblasts produce higher levels of bone morphogenic protein 2 (BMP2), a protein usually involved in development of bone and cartilage.
Ramping up BMP2 production using either genetic or recombinant protein approaches caused melanoma cells to become more invasive and resistant to targeted anticancer therapies. Conversely, blocking BMP2 production using a natural inhibitor rendered them more sensitive to anticancer therapies in both male and female mice. “The findings from these studies, the scientists noted, “supports that reducing BMP2 activity reverts melanoma tumors from a slow-cycling, invasive, therapy-resistant phenotype to a more proliferative, therapy-sensitive phenotype.” The combined results from experiments in their mutant melanoma model “… clearly show that thee differentially secreted factors within the TME can dictate therapy responses based on the age and sex of the host.”
The study has significant implications for cancer research. Currently, most preclinical cancer studies use young mice. However, the newly reported findings indicate that studying cancer in older mice and aging human cells is essential. “We also need to understand whether men and women respond differently to therapies, and better tailor their therapy to both sex- and age-related differences,” Weeraratna said. “Our data on the sex-dependent role of aging TME highlights two key points,” the authors stated. “… first, the importance of including sex and age as a variable in clinical trial design and preclinical animal models and, second, in melanoma prognosis and decision-making regarding choice of treatment modalities.”
The researchers are now studying how age- and sex-related changes in immune system cells surrounding melanoma cells affect how well the tumors respond to immune cell-boosting therapies increasingly used to treat melanoma. They would also like to study age- and sex-related changes in other cancers, including pancreatic cancer.





