A new study found that the intracellular Plasmodium parasite, which causes malaria, can be “hijacked” to deliver drugs more effectively through cholesterol uptake pathways. Researchers from the Australian National University found that the effectiveness of antimalarial drugs was enhanced when they linked these drugs to steroids that resemble the structure of cholesterol. This tactic might work for many other parasites and infections that rely on cholesterol from their hosts.
Plugging the cholesterol sink
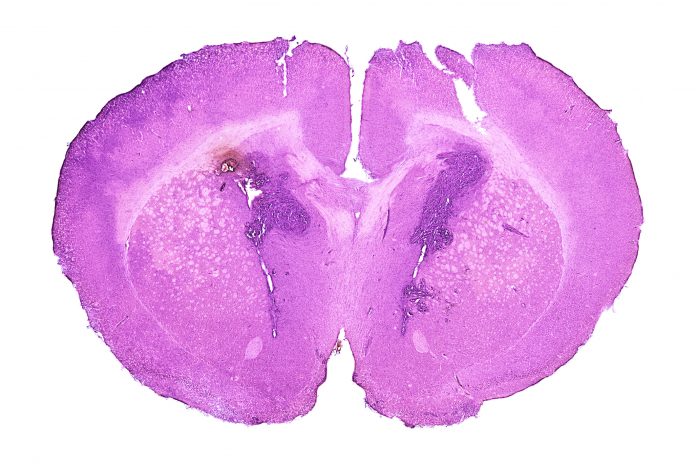
Cholesterol is an essential steroidal nutrient for the membranes of many different kinds of cells, including those in animals and even some protozoa. An essential lipid for parasite survival, neither the parasite nor its host red blood cells can synthesize cholesterol. When a parasite like Plasmodium infects a red blood cell, the cholesterol commonly found on the host cell membranes builds up inside the parasite, acting as a cholesterol sink. But if this process is interrupted, the distribution of cholesterol changes, ultimately killing the parasite.
Merryn Fraser and Blake Curtis, the study’s co-lead authors, studied cholesterol uptake into P. falciparum parasites with fluorescent cholesterol analogs, establishing that cholesterol molecules with bulky fluorescent moieties could be delivered to intracellular parasites inside human red blood cells. By replacing the fluorophore with primaquine, Fraser and Curtis created a more effective compound against three stages of the Plasmodium life cycle: the asexual intraerythrocytic, sexual gametocyte, and liver stages. The results also show that this compound has lower cytotoxic effects on human cell lines.
Additionally, Fraser and Curtis outline a method of directly altering steroids into compounds with drug-like properties by attaching peroxides directly to the steroid structure. These compounds show promise as therapeutic agents, showing greater potency than primaquine against asexual P. falciparum. However, further chemical modifications and mechanistic studies would likely be needed before this proof-of-concept drug could be used as an antimalarial. Also, substituting synthetic reactive groups for existing drugs can change the cholesterol mimic approach to make new chemicals that fight malaria.
Since many of the antimalarial drugs on the market today work best against the parasite’s asexual blood stages, this strategy may allow for the efficient targeting of these other stages with the same drug. This may eliminate the parasites in the liver before they reach the blood stages, preventing symptoms altogether or decreasing the risk of transmission to a new host by killing gametocytes. These results provide proof-of-concept that cholesterol mimics can be developed as a drug delivery system against Plasmodium parasites to improve drug efficacy and defeat drug resistance, ultimately reducing the burden of malaria.